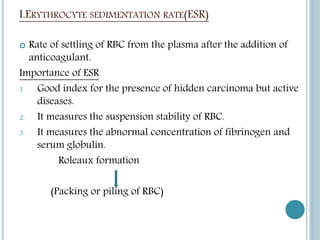
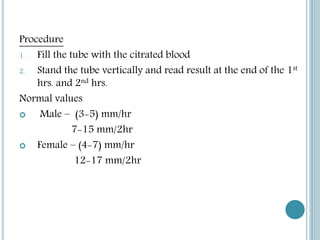
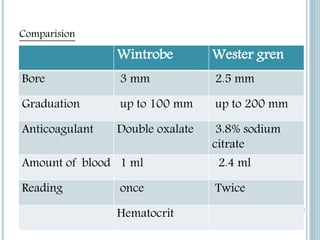
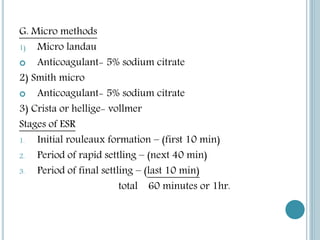
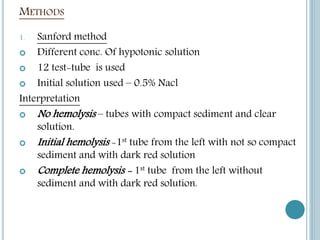
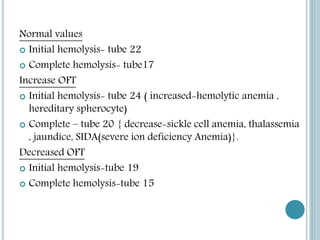
1. The document discusses various methodologies for measuring the erythrocyte sedimentation rate (ESR) and osmotic fragility test, including the Wintrobe, Westergren, and Sanford methods.
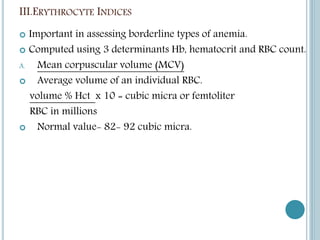
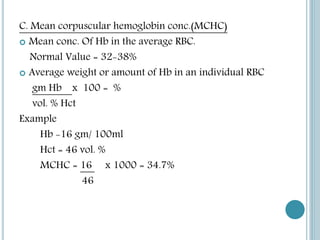
2. It also covers erythrocyte indices like MCV, MCH, and MCHC, which are computed from RBC count, hemoglobin, and hematocrit values to assess anemias.
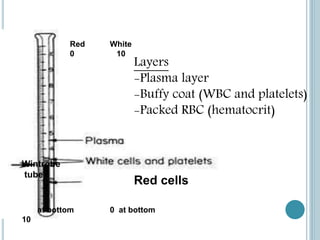
3. ESR measures the rate of settling of red blood cells and can indicate inflammatory conditions, while the osmotic fragility test examines stability of RBCs in hypotonic solutions based on hemolysis levels.