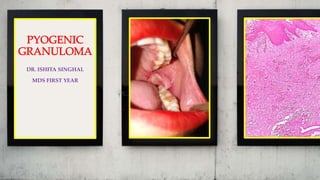
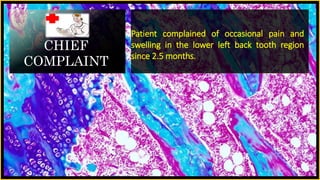
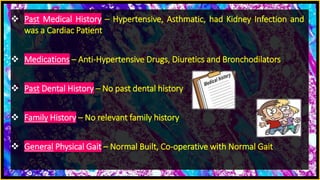
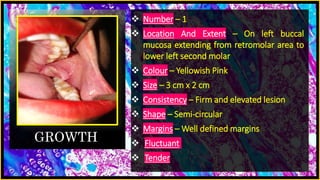
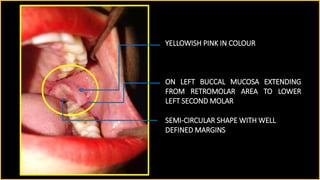
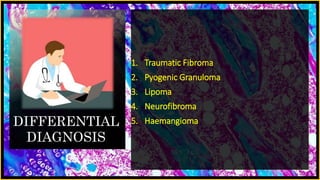
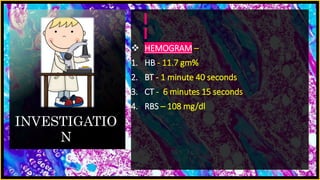
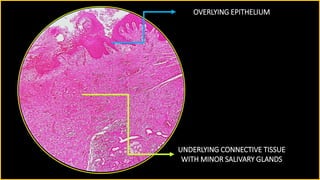
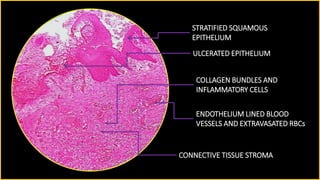
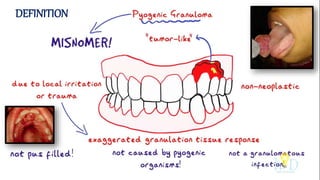
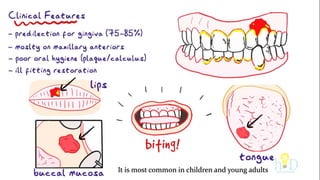
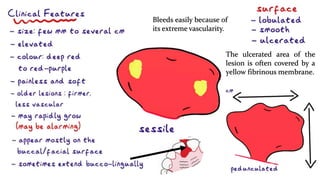
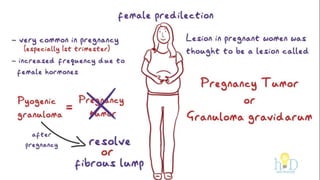
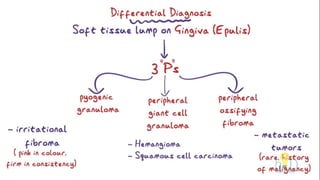
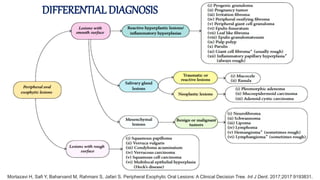
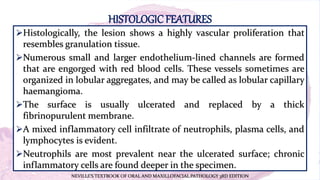
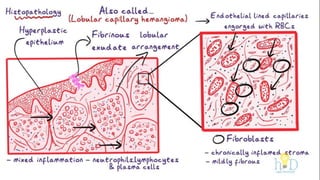
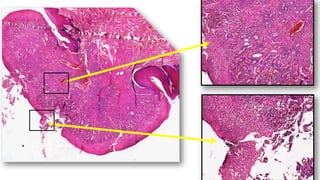
The document presents a medical case study of a 36-year-old female patient with a complaint of pain and swelling in the lower left back tooth area, diagnosed with pyogenic granuloma after an excisional biopsy. The histopathological examination showed a highly vascular proliferation resembling granulation tissue with inflammatory cells. Treatment recommendations include surgical excision of the granuloma and removal of irritants.