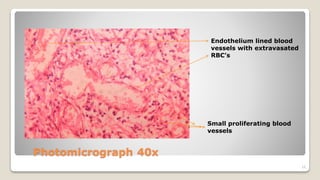
This case report describes a pyogenic granuloma lesion in a 30-year-old female patient. She presented with a 3-month history of a painless gingival swelling interfering with eating and speaking. Clinical examination revealed an oval-shaped, erythematous nodule measuring 0.7 cm. Histopathological examination showed numerous blood vessels with extravasated red blood cells within the connective tissue, along with inflammatory cells. This was consistent with a diagnosis of pyogenic granuloma. The lesion was surgically excised. Pyogenic granuloma is a common gingival growth considered to be an exaggerated response to minor trauma or irritation.