- Diseases of the pulp and periapical tissues can result from caries, trauma, or other injuries that lead to inflammation and necrosis. This summary will discuss pulpitis, periapical diseases, and osteomyelitis.
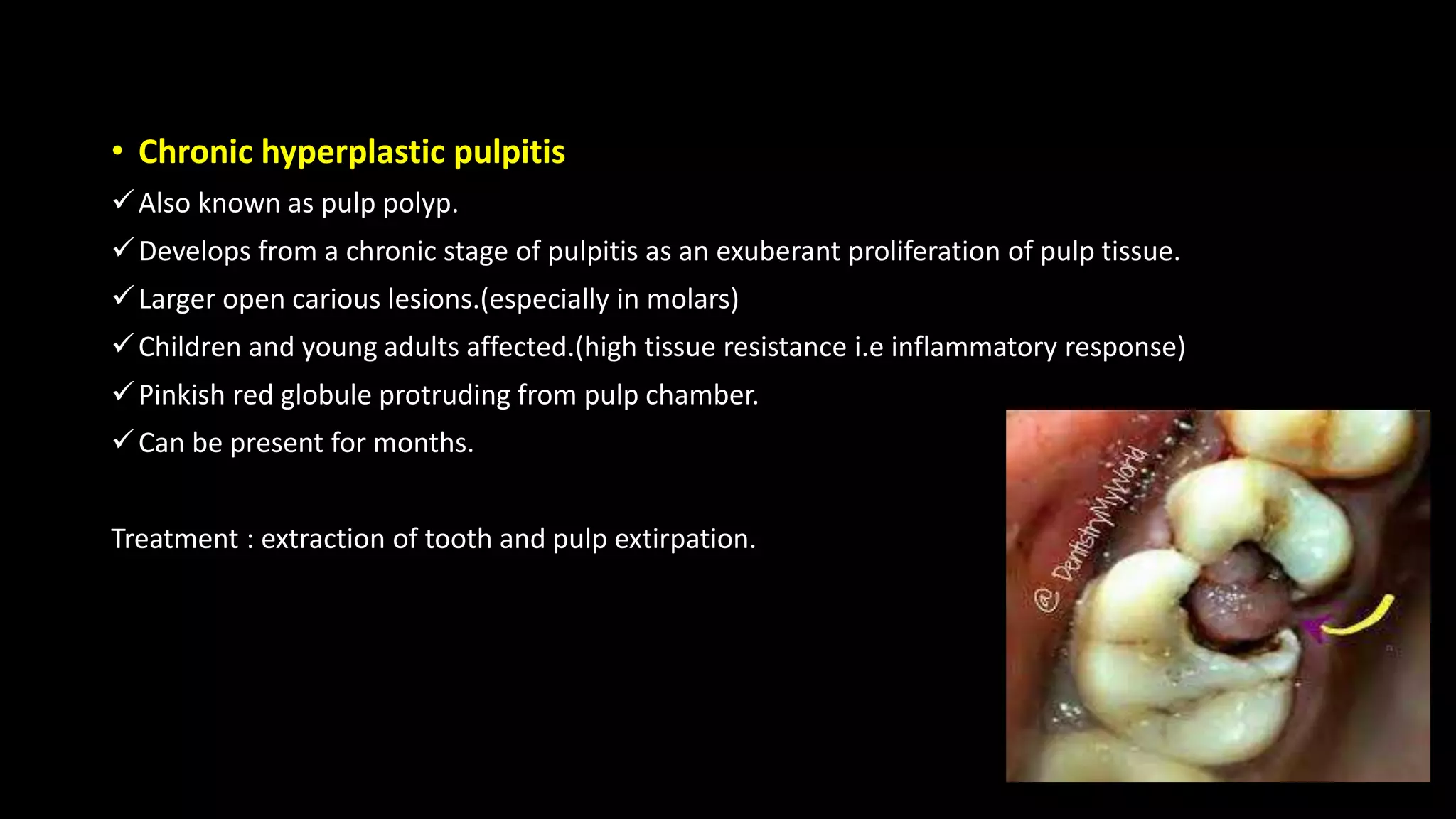
- Pulpitis can be focal/reversible, acute, or chronic and results from inflammation of the pulp in response to injuries or irritants. Acute pulpitis causes severe pain while chronic pulpitis may be asymptomatic.
- Periapical diseases like apical periodontitis, periapical granulomas, cysts, and abscesses occur when inflammation spreads from the pulp through the root canals into surrounding tissues. Left untreated, periapical abscesses