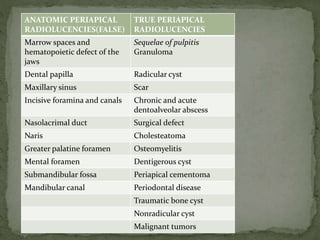
Periapical radiolucencies
- 1. ANATOMIC PERIAPICAL RADIOLUCENCIES(FALSE) TRUE PERIAPICAL RADIOLUCENCIES Marrow spaces and hematopoietic defect of the jaws Sequelae of pulpitis Granuloma Dental papilla Radicular cyst Maxillary sinus Scar Incisive foramina and canals Chronic and acute dentoalveolar abscess Nasolacrimal duct Surgical defect Naris Cholesteatoma Greater palatine foramen Osteomyelitis Mental foramen Dentigerous cyst Submandibular fossa Periapical cementoma Mandibular canal Periodontal disease Traumatic bone cyst Nonradicular cyst Malignant tumors
- 2. TRUE PERIAPICAL RADIOLUCENCIES represents lesions that are truly located in contact with apex of a tooth Their shadow cannot be shifted from the periapex by taking additional radiographs at different angles • FALSE PERIAPICAL RADIOLUCENCIES Are produced by anatomic cavities or lytic bony lesions that donot contact the apex of a tooth The radiolucent shadows may be shifted from the periapex by taking additional radiograph at different angles
- 5. SUBMANDIBULAR GLAND FOSSA GREATER PALATINE FORAMEN
- 8. Most common type Result of a successful attempt by the periapical tissues to neutralize and confine the irritating toxic products(prostaglandins,kinins,lysosomes and endotoxins)that are escaping from the root canal Low grade inflammation Microstructure consists of proliferating endothelial cells,capillaries,young fibroblasts,a minimal amount of collagen and chronic inflammatory cells FOUR TYPES ON BASIS OF HISTOPATHOLOGY Exudative Granulomatous Granulofibrous fibrous
- 9. Radiographically,lesion is a rather well circumscribed radiolucency somewhat rounded in shape and surrounding the apex of the tooth May or may not have a thin radiopaque(hyperostotic)border. Radiographs reveal presence of deep restorations,extensive caries,fractures or a narrower pulp canal Periapical radiolucency of diameter less than 1.6cm is considered as periapical granuloma Electrical and thermal pulp testing will usually indicate that pulp is non-vital
- 10. Tooth is completely asymptomatic Absence of sensitivity to percussion Crown may have darker colour than of its neighbours because of blood pigments that have diffused into empty dentinal tubules Swelling and expansion of cortical plate is unusual since they rarely reach a size to produce such an effect
- 11. GRANULOMA Small round or oval radiolucency <1.6cm in diameter surrounding apex of tooth with or without well-circumscribed borders
- 12. Second most common Inflammatory cyst Origin from cell rest of Malassez Orginate in pre-existing periapical granuloma As the masses of proliferating epithelial nests increase in size, the central cells start to degenerate and liquefy Leads to liquid-filled cavity lined with epithelium Cysts continues to grow because of a combination of factors 1. The products from the cell lysis are probably irritating and may provide growth stimulus 2. Epilthelial cells discharged into the cyst lumen increase the protein content and hence the osmotic pressure of cyst
- 13. fluid leading to more water diffusion into lumen 3. The pressure exerted by the enlarging cyst on the alveolar bone induces osteoclastic action and resorption of the periapical bone FEATURES The more pronounced the hyperostotic border of the lesion, the more likely is the lesion to be a cyst Should measure atleast 1.6cm in diameter An untreated cyst may slowly enlarge and cause expansion of cortical plates,observed clinically as dome like swelling on the alveolus over the periapical region of involved tooth
- 14. The swelling may develop on either the buccal or lingual side of alveolar process and will be covered with normal-appearing Mucosa Initially,bony hard to palpation,but later it may demonstrate A crackling sound(crepitus) as cortical plates become thinned Usually,the cortical plates remain intact Large cysts may involve a complete quadrant with some of the Teeth occasionally mobile and some of the pulps non-vital Root resorption is also seen the causative tooth and the alveolar swelling are painless in case of sterile cysts,however when infected develops pain
- 15. RADICULAR CYST Round or oval well- defined radiolucency >1.6cm in diameter
- 16. Well defined radiolucency at apex of untreated asymptomatic tooth with nonvital or diseased pulp:90% cases dental granuloma or radicular cyst(1.6cm or more=radicular cyst) PERIAPICAL SCAR: if well sealed, persistent asymptomatic nonenlarging radiolucency associated with teeth which received non-surgical endodontic treatment for granuloma and cyst Asymptomatic radiolucency persisting after root resection can be either a scar or surgical defect PERIAPICAL CEMENTOMA: pulp is vital and mostly involve lower teeth ,mostly incisors TRAUMATIC BONE CYST :pulp is vital and 90% occurs in mandible(molar,premolar,incisor region)
- 17. Extraction Conservative root canal therapy Cyst respond well to nonsurgical endodontic treatment:2 theories 1. Instrumentation beyond apex permits the cyst to drain into canal 2. When root canal is sealed the irritating products from gangrenous pulp are no longer present and inflammation subsides Biopsy via buccal window to determine the nature of lesion Apical curettage or root resection procedure if 2cm or larger(radicular cyst) Retrograde filling and periapical curettage if root canal is nonnegotiable
- 18. For large radicular cysts with considerable bone loss Surgical enucleation Restoration of defect with graft,preferably autogenous bone Marsupialization Decompression Decompression with delayed enucleation Creation of common chamber with maxillary sinus or nasal cavity Sequential post surgical radiographs to ensure regression of defect
- 19. Composed of dense fibrous tissue Situated at periapex of a pulpless tooth in which rootcanals have been filled Represented by granuloma,cyst or abscess whose healing has stopped in the formation of dense scar tissue(cicatrix) rather than bone In some instances,granulation tissue during resolution slowly organizes with production of more collagen fibers leading to dense collagenous connective tissue scar :permanent and radiolucent Microscopically : few spindle shaped fibroblasts scattered throughout dense collagen bundles Scarring periapical granuloma: relatively young ,less dense scar experiencing intermittent inflammation
- 20. Well circumscribed radiolucency that is more or less round resembling granuloma and cyst radiographically but usually smaller Asymptomatic Occurs mostly in anterior region of maxilla Majority of involved teeth have been endodontically treated MANAGEMENT No treatment required
- 21. SCAR Well defined borders Remain constant in size over years asymptomatic
- 22. Primary or neoteric abscesses: associated with teeth that have not developed apparent radiolucent lesion • Acute apical periodontitis/acute periapical abscess Secondary or recrudescent abscesses: develop in a previously existing asymptomatic periapical radiolucent lesion PRIMARY ABSCESS: Radiographically normal periapical region Occurs due to rapid spread of virulent bacteria from canal to periapical tissues Very sensitive tooth and perhaps alveolar swelling No resorption of bone due to sudden onset and course Frequent swelling of the periodontal ligament which force the tooth out slightly from its socket leading to an increased periodontal ligament space around entire root
- 23. Chronic or acute type depending on 1. Number and virulence of invading organism 2. Resistance of host 3. Type and timing of treatment MICROORGANISMS: Streptococci,Staphylococci, Bacteroides, Peptococcus, Peptostreptococci, Actinomyces, Eubacterium, Fusobacterium
- 24. RADIOGRAPHIC periapical radiolucency is a feature of secondary abscess Radiolucency may vary in size Depending on duration ,acuteness and chronicity,margins may be well defined with hyperostotic border to poorly defined in chronic cases Sometimes present as blurred area of lessened density than surrounding bone Deep restorations, caries, narrowed pulp chamber or canals : suggestive of non-vital pulp Roots may show resorption of apex
- 25. APICAL ABSCESS Diffuse radiolucency in periapical region of affected tooth
- 26. MICROSCOPICALLY Central region of necrosis with dense accumulation of PMN leukocytes surrounded by inflamed connective tissue wall of varying thickness CLINICALLY Very painful to percussion No response to electric pulp tests Ice application relieves pain while heat aggravates the pain Progression leads to penetration of cortical plates, formation of space infection and sinus tracts Warmth of overlying skin or mucosa Elevation of systemic temperature
- 27. A small proliferation of granulomatous tissue often forms on the surface referred to as parules pain subsides when drainage is established COMPLICATIONS Osteomyelitis Septicemia Septic emboli Ludwig’s angina Cavernous sinus thrombosis
- 28. Drainage established by opening pulp chamber and passing file through canal into periapical region If not possible,TREPHINATION procedure done:opening made through mucosa and bone to abscess at apex A THROUGH AND THROUGH DRAIN may be placed in abscess in case of vestibular and lingual space infection along with frequent irrigation with H2O2 solution and saline sample of pus for culture and sensitivity test Penicillin therapy(not less than 500mg qid for atleast 5 days)/erythromycin Antibiotics before extraction In case of draining sinus,exact location of the abscess can be located by inserting a gutta-percha cone to the extent of sinus and making radiograph of that area
- 29. Occurs in patients with periapical abscess with underlying systemic disease or who have received large doses of radiation therapy Defined as an infection of bone that involves all 3 components: periosteum, cortex, and marrow Osteitis: localized ; Osteomyelitis: diffuse ACUTE OSTEOMYELITIS: Similar to acute primary alveolar abscess, rapid onset and course, no bone resorption, thus radiolucency may not be present CHRONIC OSTEOMYELITIS: low –grade infection of bone if untreated leads to extensive bone destruction,produces radiolucent lesion
- 30. Chronic osteomyelitis demonstrate 4 distinct radiographic picture 1. Completely radiolucent 2. Mixed radiolucent and radiopaque 3. Completely radiopaque 4. Garre’s osteomyelitis FEATURES Seldom observed in maxilla because of rich blood supply Tooth associated: non-vital pulp,may be sensitive to percussion and previously associated with periapical abscess Periapical radiolucency somewhat rounded in shape with poorly defined and ragged borders
- 31. Sequestrum present as radiopacity within a radiolucency Draining tract may be seen as radiolucency through cortical plate beneath sinus opening on mucosa or skin Fever,malaise Swelling on bone and mucosa around osteomyelitis
- 33. If area of bone destruction is large and region is not painful:Eosinophilic granuloma:biopsy If only alveolar portion of jawbone is infected:Alveolar abscess If tooth suspected is in fracture line or if an uncontrolled systemic disease is present: Chronic Osteomyelitis Paget’s disease: several bones with classic wool appearance MANAGEMENT Best treatment will be to extract the offending tooth rather than conserving it by endodontic procedure
- 34. Arise from elements in periodontal ligament Other names: 1. Periapical cemental dysplasia 2. Periapical osteofibroma 3. Periapical osteofibrosis Arise on a reactive basis rather than on neoplastic basis 3 stages in their development which are radiographically apparent
- 35. 1. Early (osteolytic or fibroblastic)stage: radiolucent 2. Cellular fibroblastic stroma with small foci of calcified material 2. Intermediate stage: radiolucent area containing radiopaque foci 3. Final stage(mature lesion):well-defined solid ,homogeneous radiopacity surrounded in most cases by thin radiolucent border Calcified material may cementum,bone or both(differentiated using polarising microscopy) FEATURES In early stage ,they occur as radiolucencies that are somewhat rounded,have well-defined borders and are associated with teeth having vital pulp
- 36. Blacks are commonly affected 80% occur in women 90% occur in mandible Asymptomatic Seldom exceeds 1 cm in diameter MANAGEMENT Treatment required only if radiographic changes present If infection or expansion of cortical plate: Surgical enucleation If inflammation of pulp:conservative endodontic treatment
- 37. 1. Hemorrhagic bone cyst 2. Extravasation cyst 3. Simple bone cyst 4. Progressive bony cyst 5. Blood cyst FALSE CYST(no epithelial lining) Localized aberration in normal bone remodeling or metabolism
- 38. FEATURES A history of trauma may or may not be present Asymptomatic except when it reaches size sufficient to cause expansion of jaws Well-defined cyst-like radiolucency above the mandibular canal either round and positioned somewhat symmetrically about periapex of root OR More elongated and oriented mesiodistally extending superiorly between premolar and molar roots producing scalloped appearance No aspiration results but sometimes serosanguineous fluid or some blood may be obtained Mandible>Maxilla Premolar-molar region most common location
- 39. TREATMENT 1. open the area surgically 2. Establish a diagnosis of traumatic bone cyst 3. Remove the tissue debris present 4. Curette the walls of bony cavity to induce bleeding 5. Close the soft tissue flap securely Antibiotics ALTERNATE METHOD:injecting venous blood into bony defect(good results but objected because sometimes in periodic radiographic follow-up examination, the radiolucency is found to be expanding)
- 41. WOOD AND GOAZ BASIC ORAL RADIOLOGY: ANIL GOVINDRAO GHOM