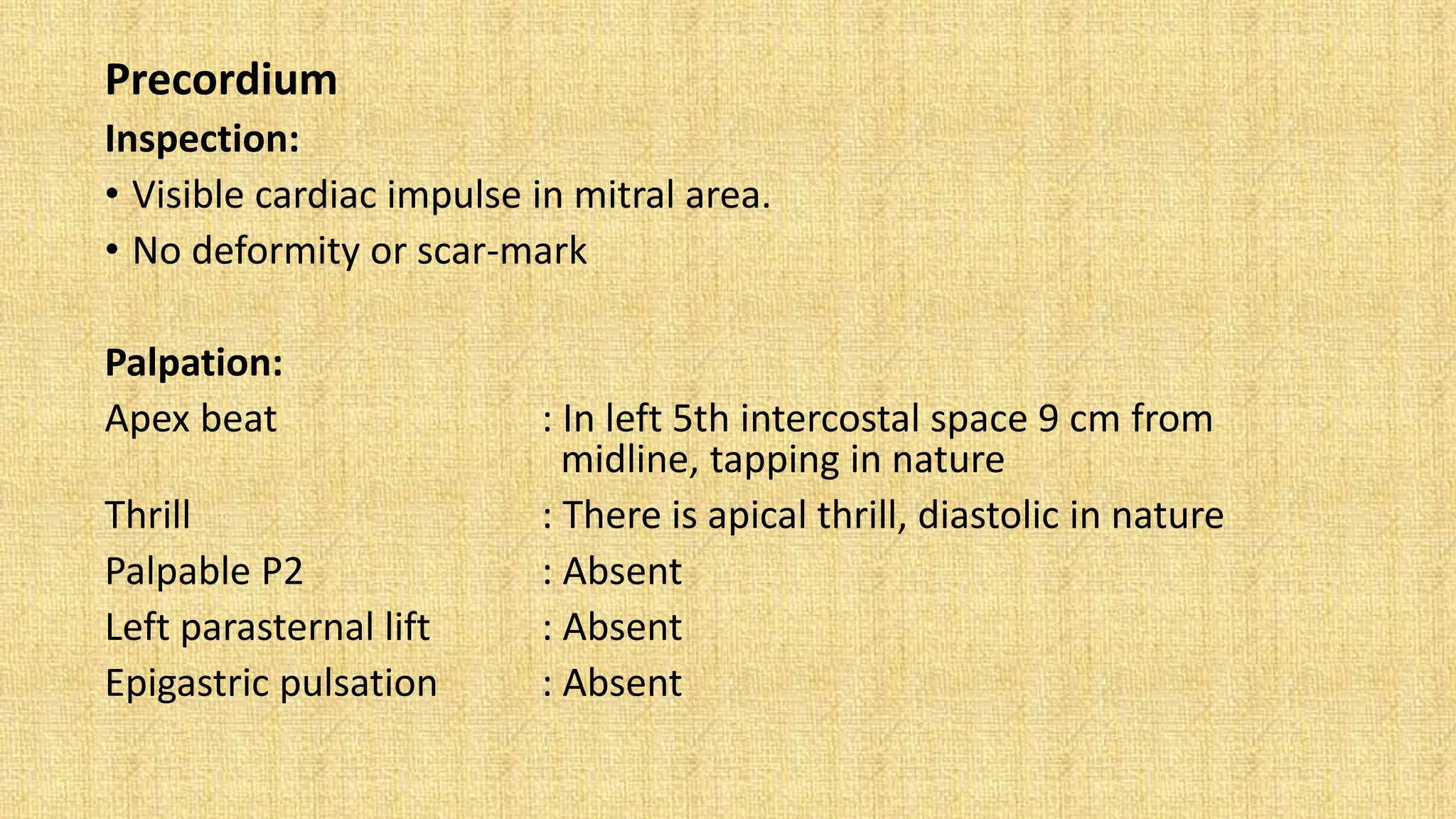
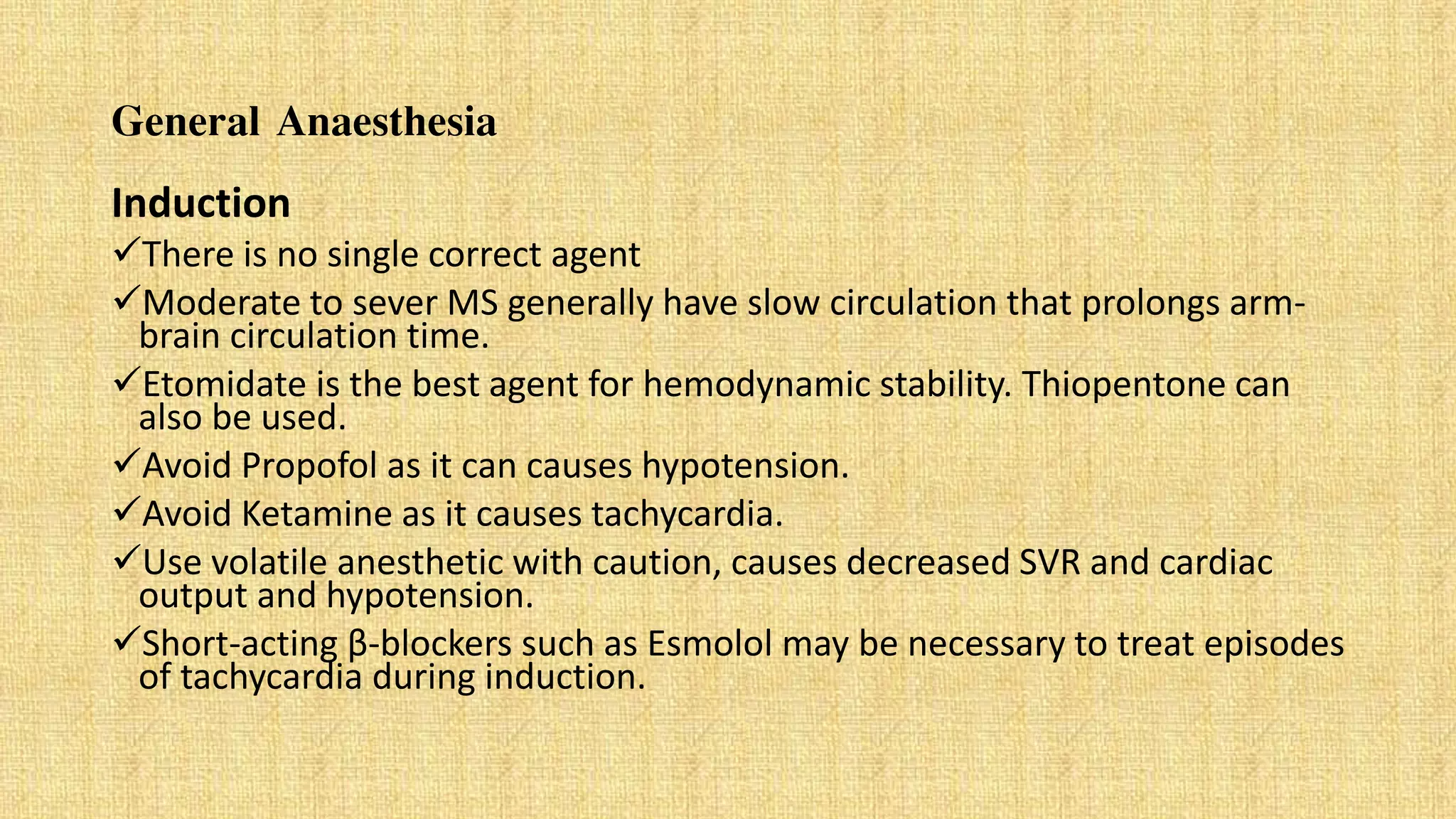
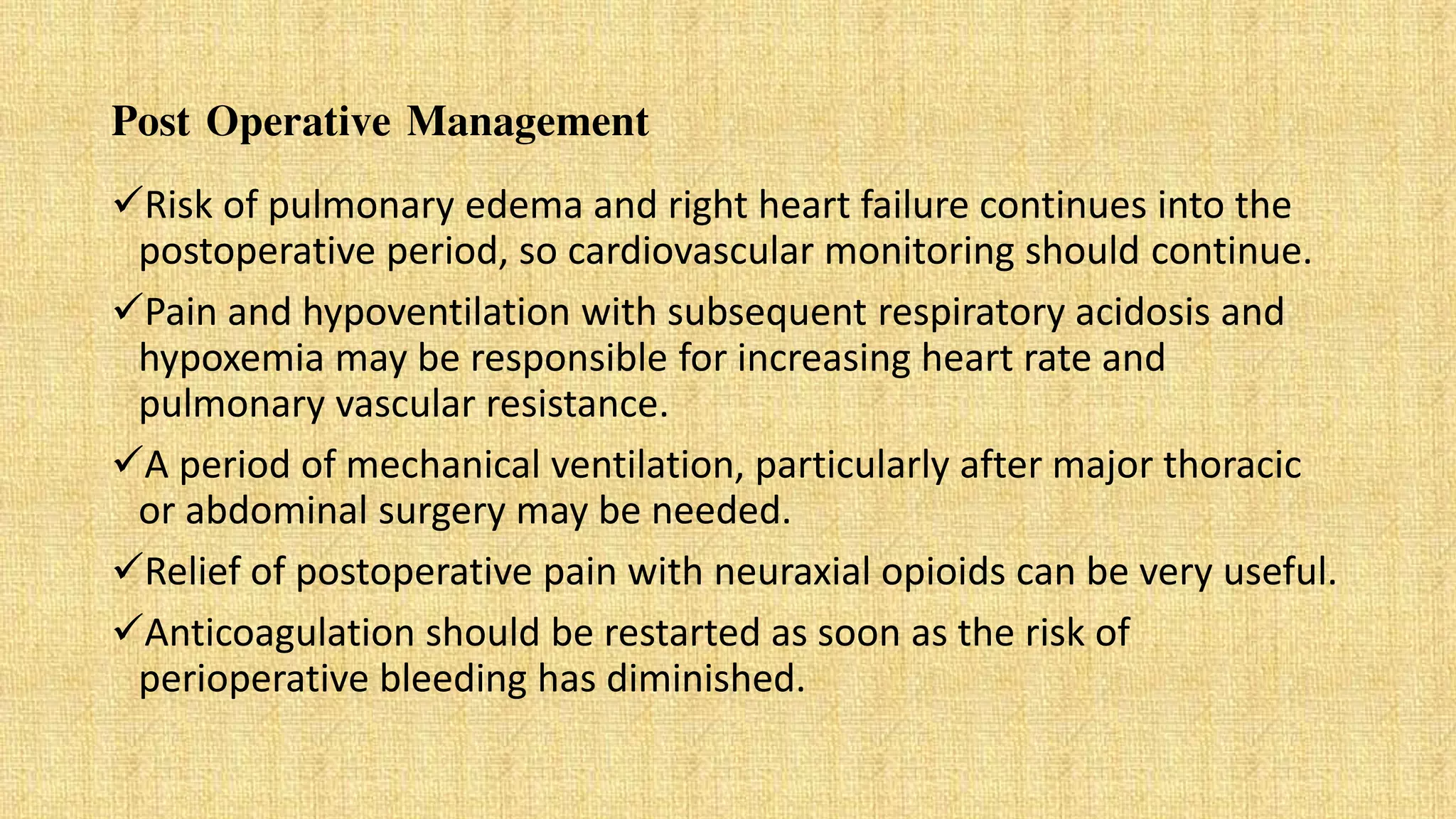
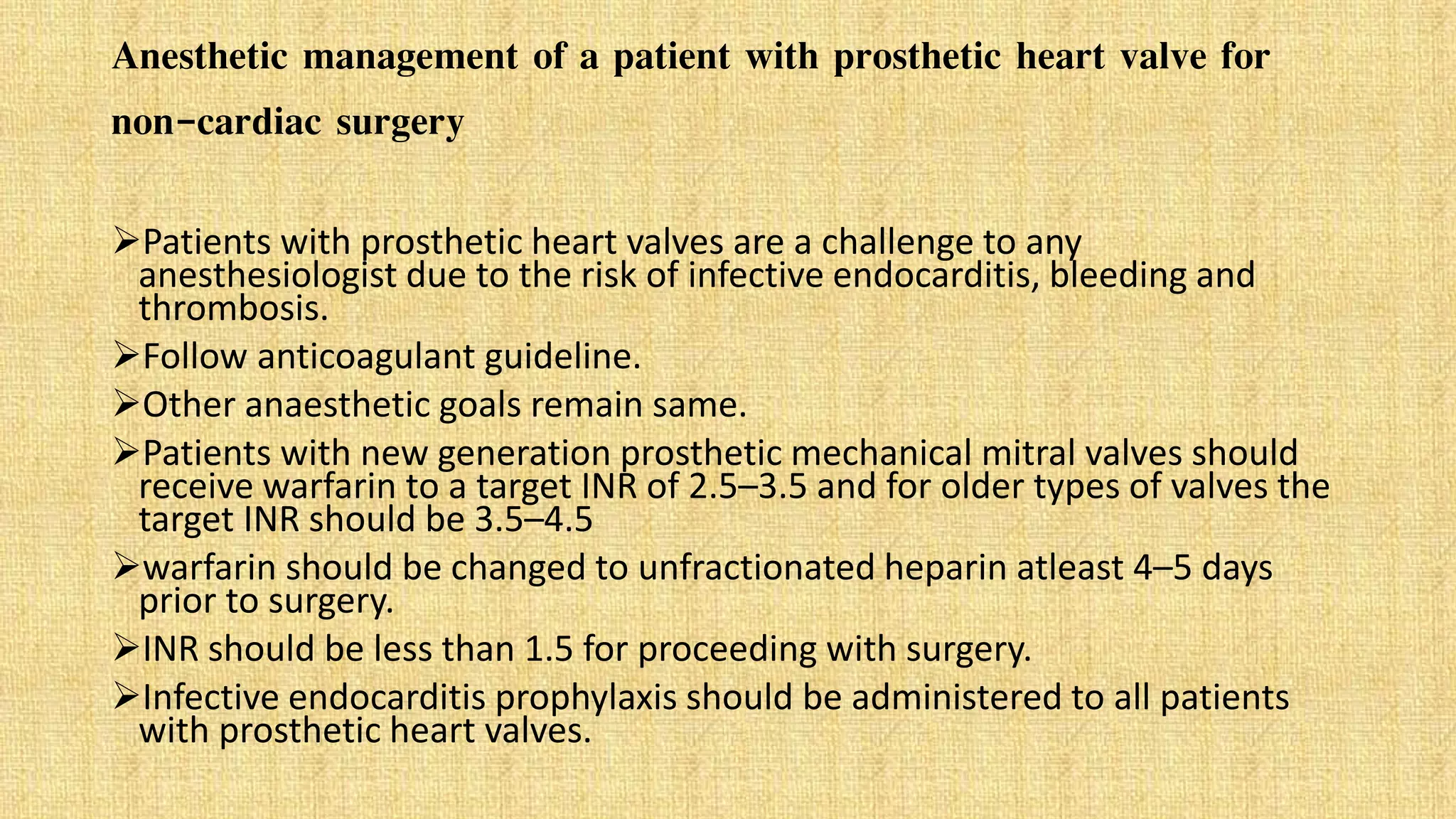
The document presents a clinical case of a 22-year-old female student diagnosed with mitral stenosis, characterized by symptoms such as breathlessness, palpitations, and a productive cough. The patient's history includes rheumatic fever in childhood, and examinations reveal acute signs of mitral stenosis along with relevant diagnostic measures including ECG and echocardiogram. Treatment options span from medical management for milder cases to surgical interventions for severe mitral stenosis, including considerations for anesthetic management during surgery.