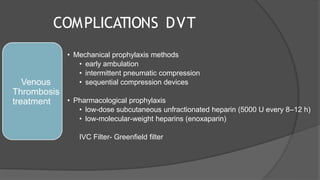
This document provides an overview of pulmonary considerations and complications in neurosurgery patients. It discusses anatomy, physiology, pulmonary care including intubation and ventilation. It also examines postoperative pulmonary complications such as pneumonia, atelectasis, respiratory failure, pulmonary embolism, and neurogenic pulmonary edema. Risk factors, pathogenesis, definitions, clinical scoring systems, and management approaches are described for various complications. Specific mechanical ventilation-related issues like ventilator-associated pneumonia are also outlined.