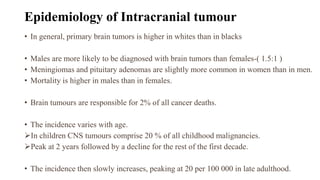
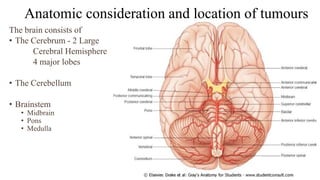
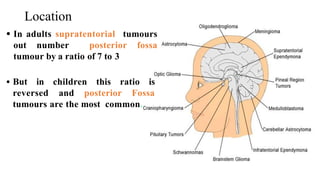
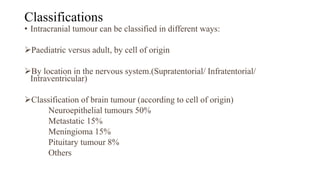
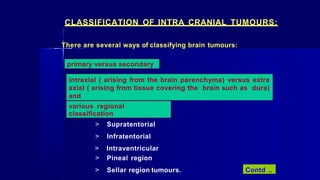
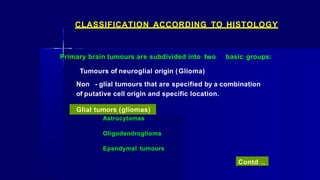
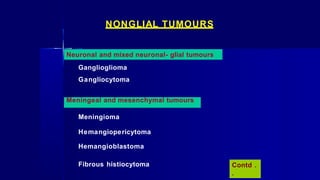
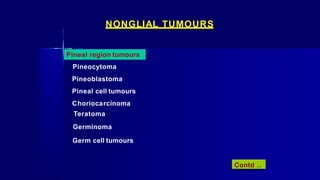
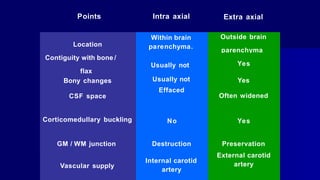
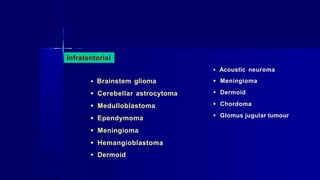
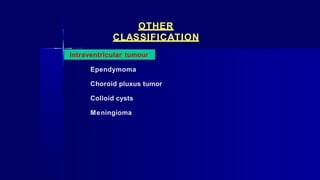
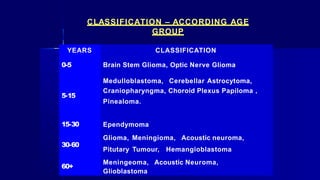
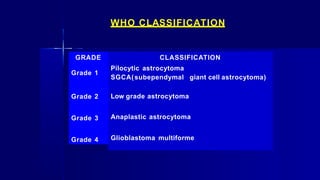
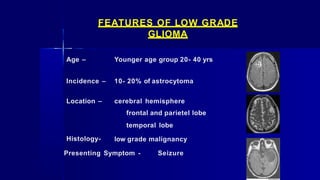
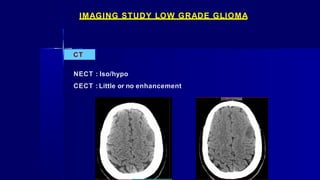
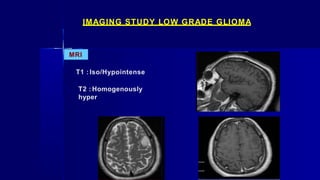
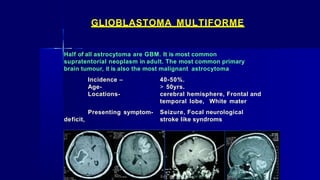
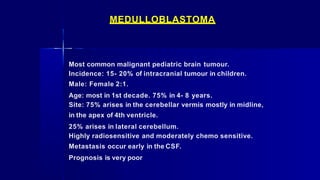
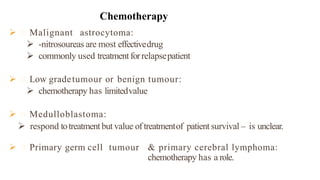
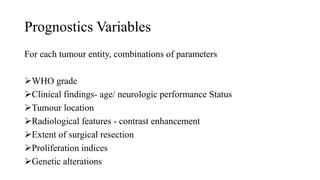
The document provides a comprehensive overview of brain tumors, discussing their epidemiology, classification, anatomical considerations, clinical features, and treatment modalities. It emphasizes the differences in tumor incidence between genders and age groups, detailing the types of brain tumors, including primary and secondary, and their histological characteristics. Recent advances in treatment approaches such as surgery, radiation therapy, and chemotherapy are also highlighted, reflecting on the multidisciplinary strategies required for effective management of these conditions.