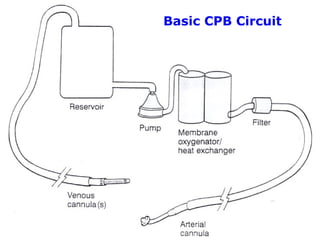
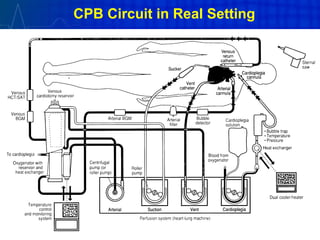
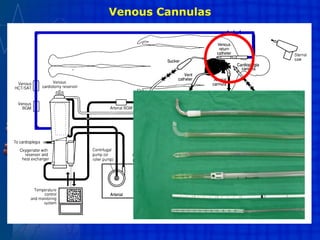
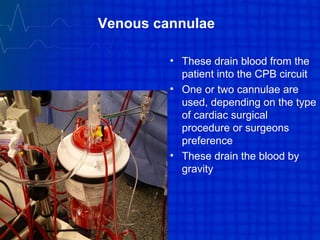
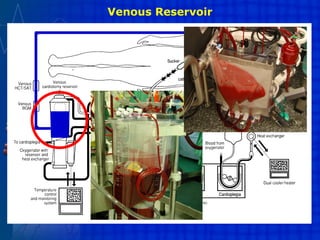
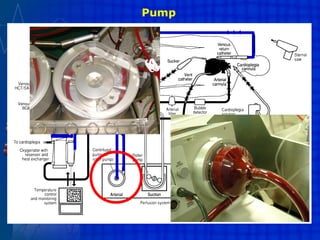
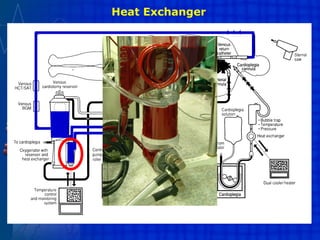
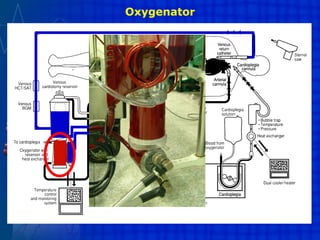
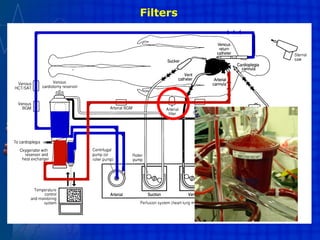
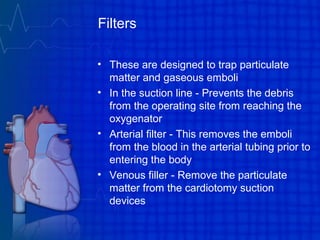
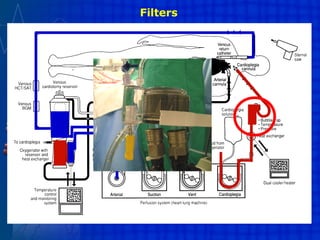
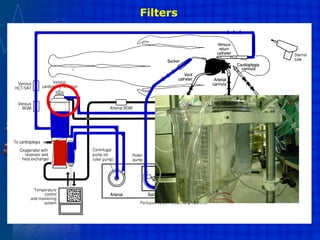
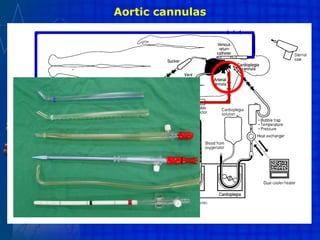
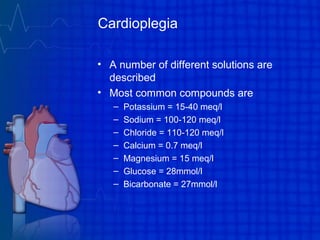
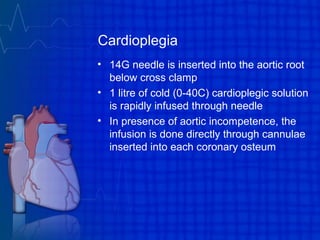
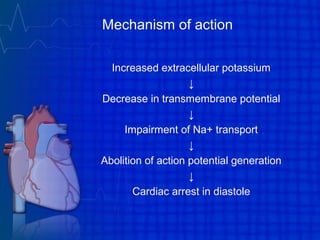
This document discusses extracorporeal circulation, specifically cardiopulmonary bypass (CPB) used during open heart surgery. It describes the basic CPB circuit including components like the venous cannula, reservoir, pump, heat exchanger, oxygenator, and arterial cannula. It outlines the steps of CPB including priming, anticoagulation, cannulation, initiating bypass, maintenance on bypass, weaning from bypass, and potential complications. CPB temporarily takes over the functions of the heart and lungs to provide a still, bloodless field for cardiac surgery using mechanical devices placed outside the body.