This document summarizes a presentation on posttraumatic stress disorder (PTSD) given by Dr. David Eisenman. Some key points:
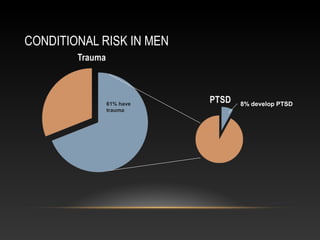
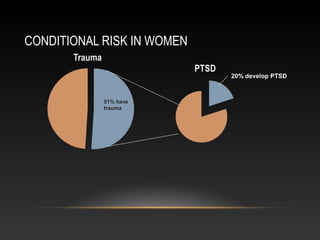
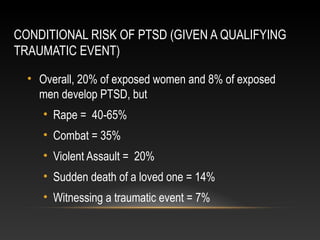
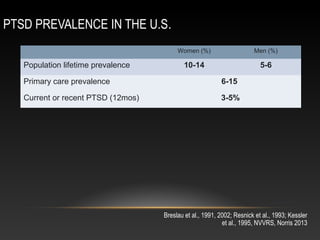
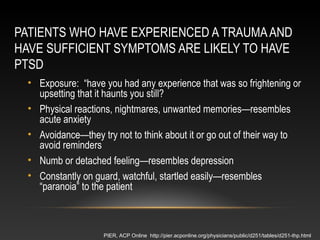
- Around 55% of US adults experience a traumatic event in their lifetime, but only 8-20% of those exposed develop PTSD depending on gender and type of trauma.
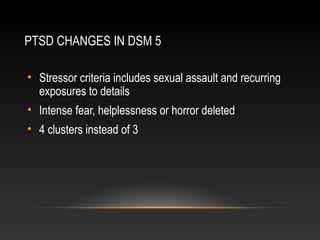
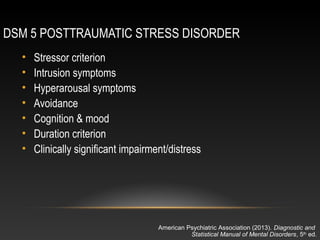
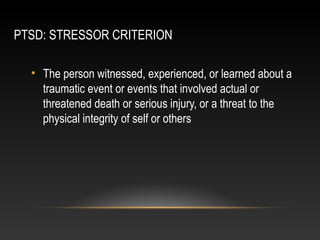
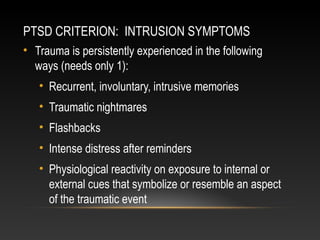
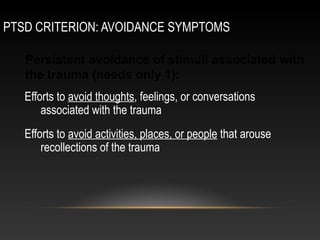
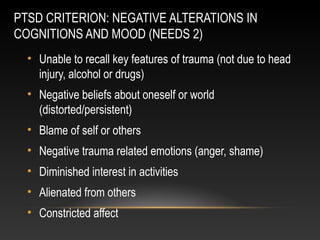
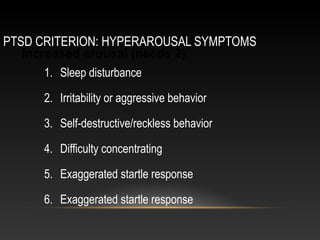
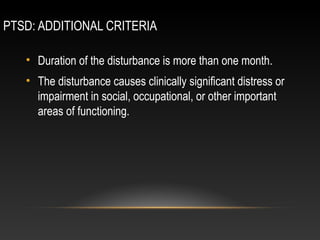
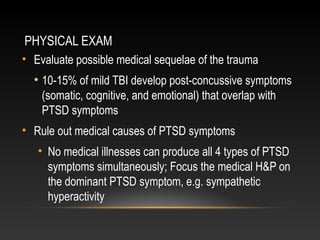
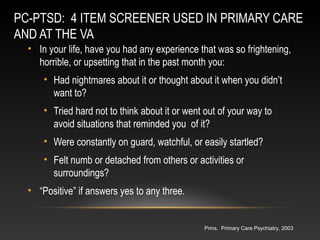
- PTSD is characterized by intrusive memories, avoidance, negative alterations in mood/cognition, and hyperarousal. The DSM-5 made some changes to these criteria.
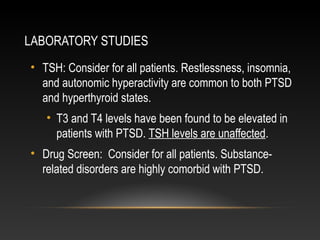
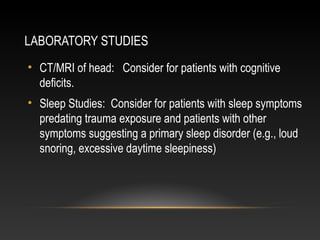
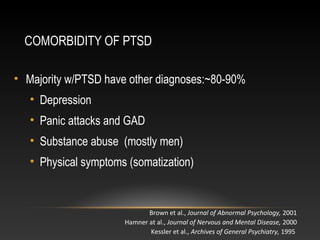
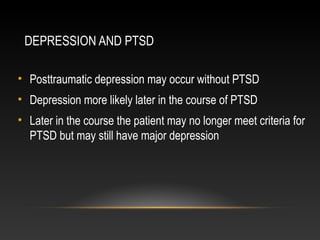
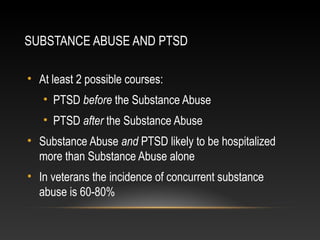
- PTSD commonly co-occurs with depression, substance abuse, and physical symptoms. It is important to assess for these comorbidities.
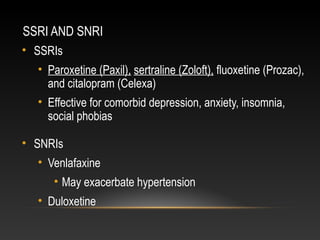
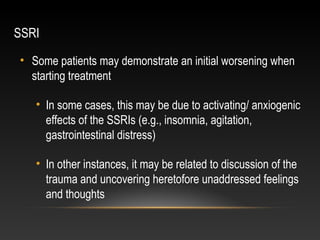
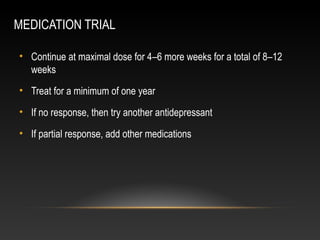
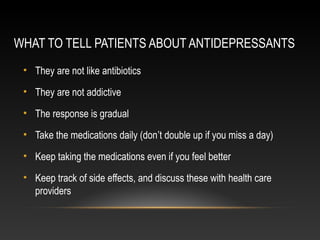
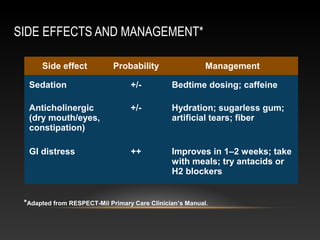
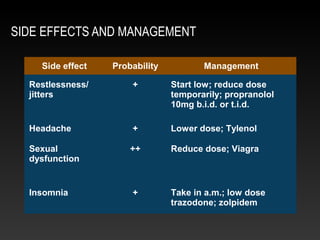
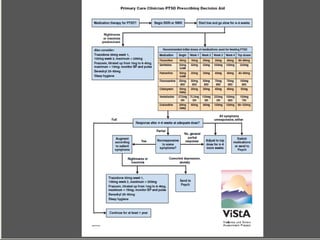
- First-line treatment involves SSRIs or SNRIs. Psych