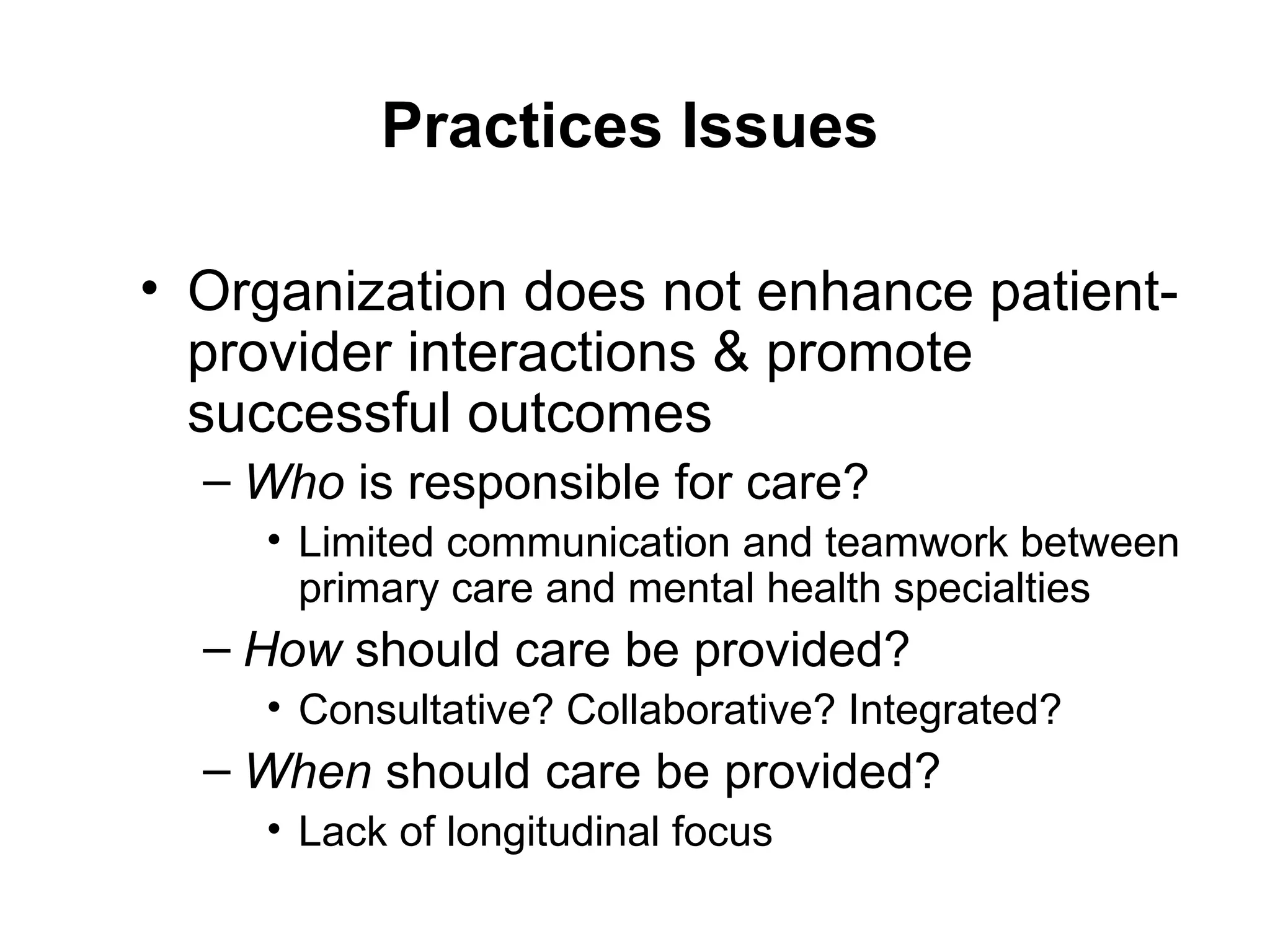
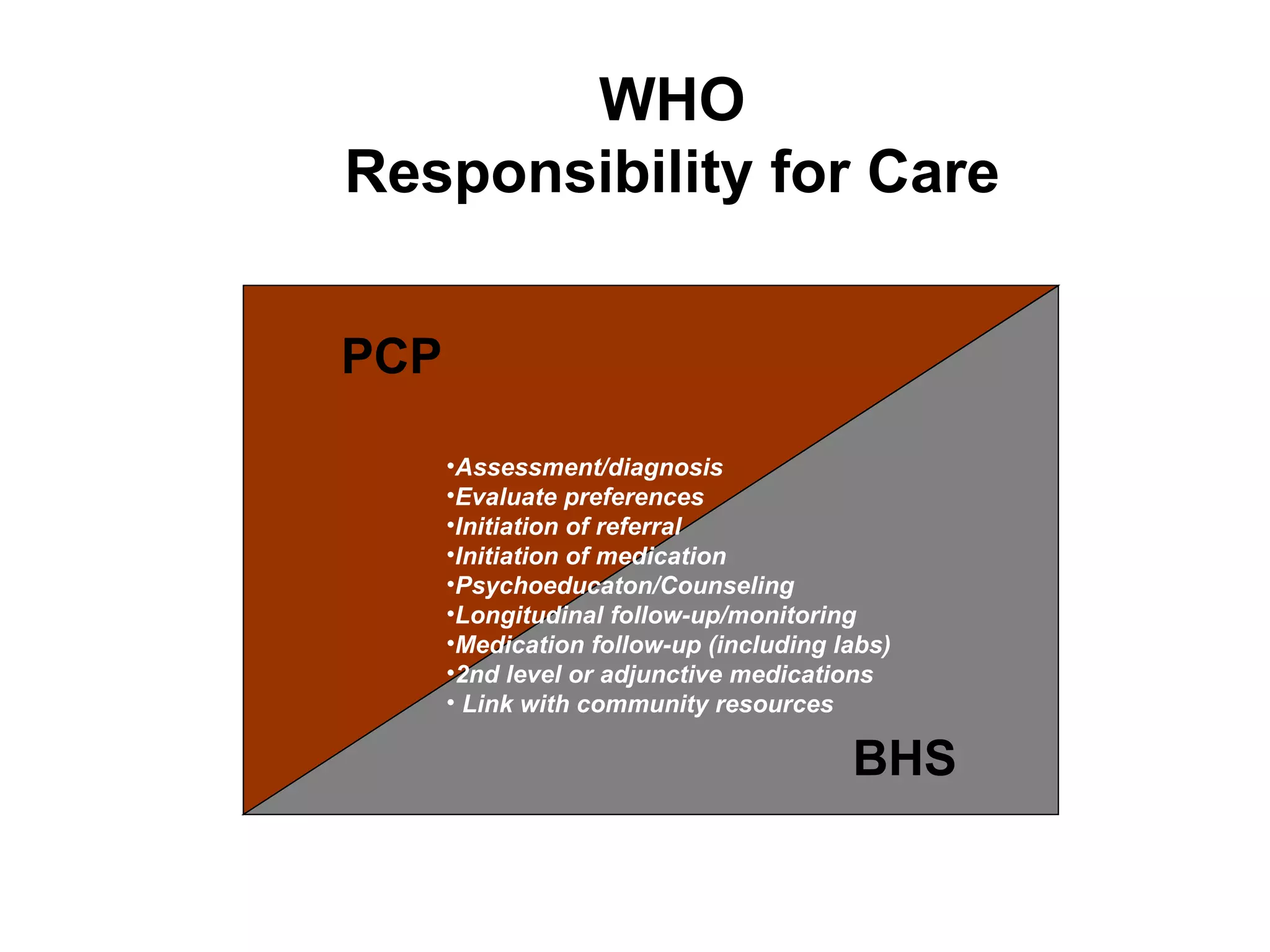
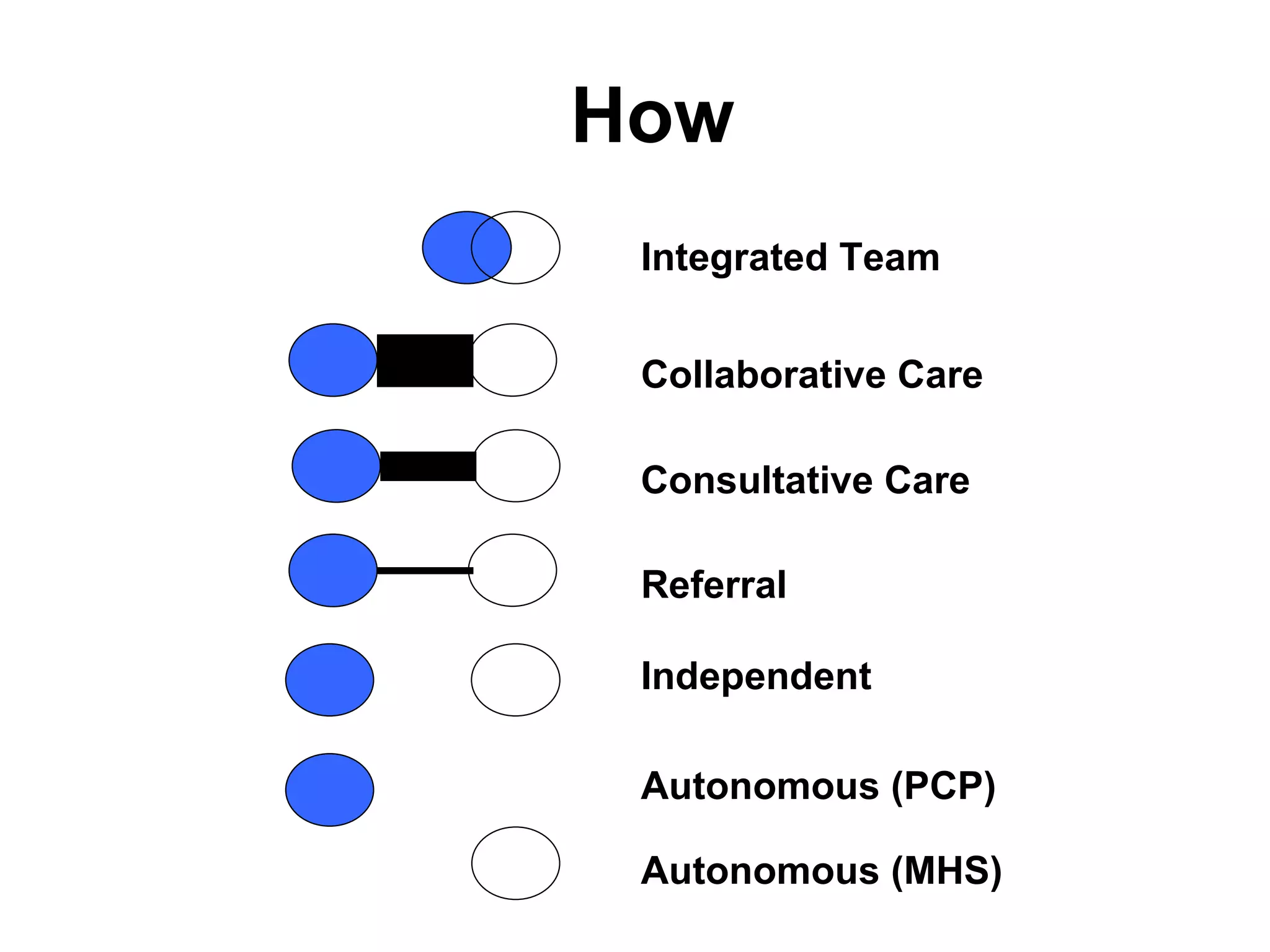
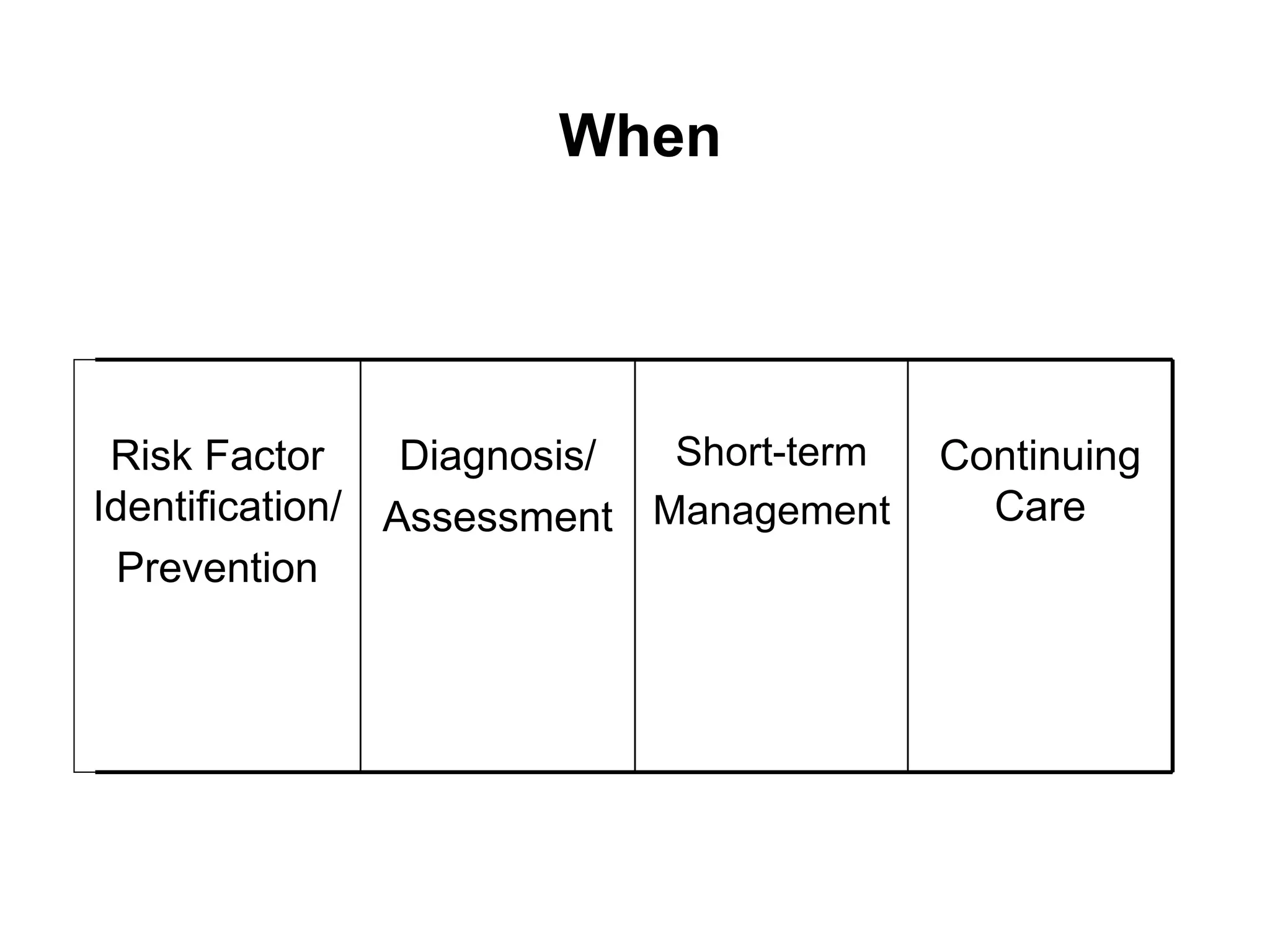
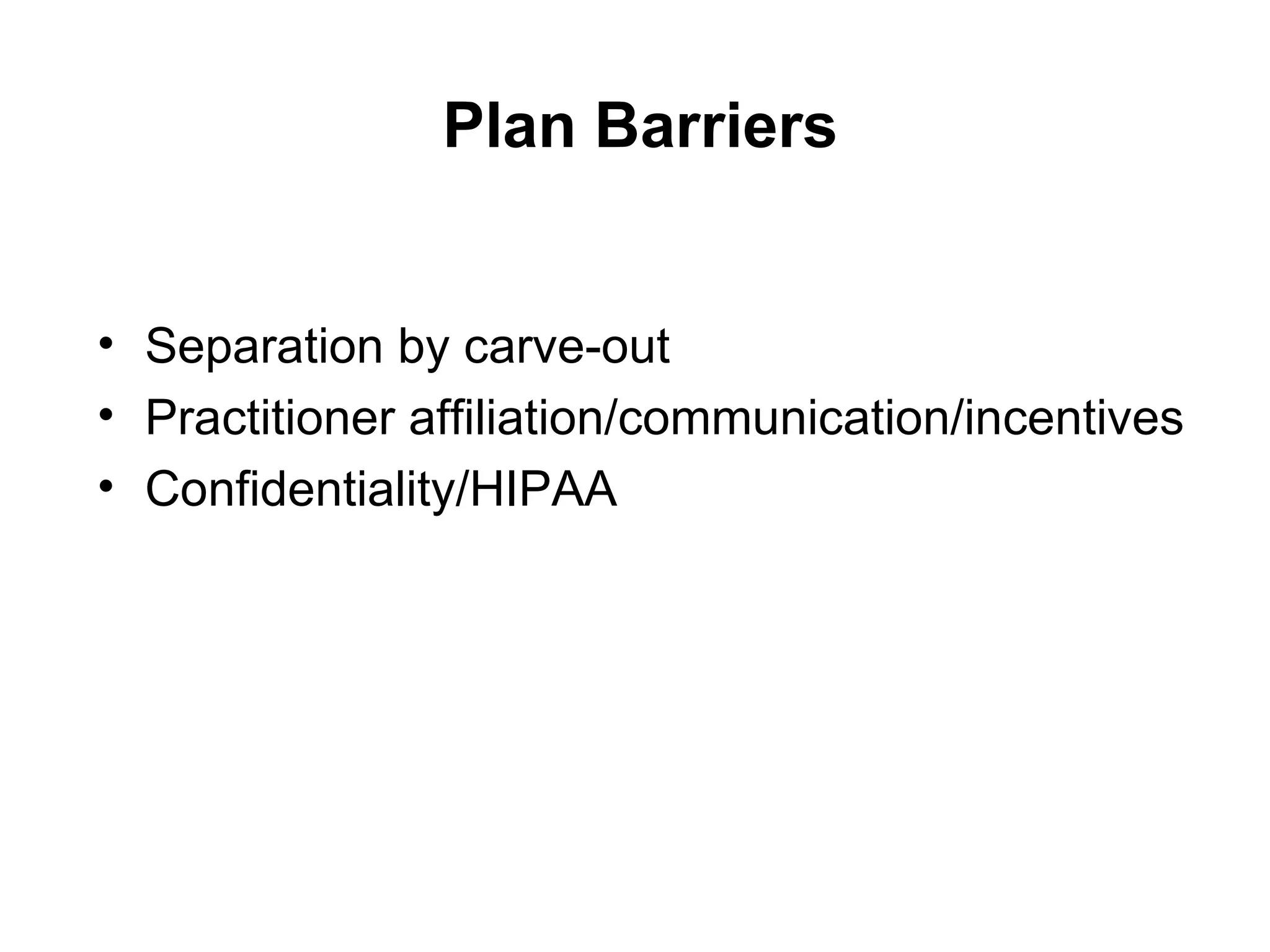
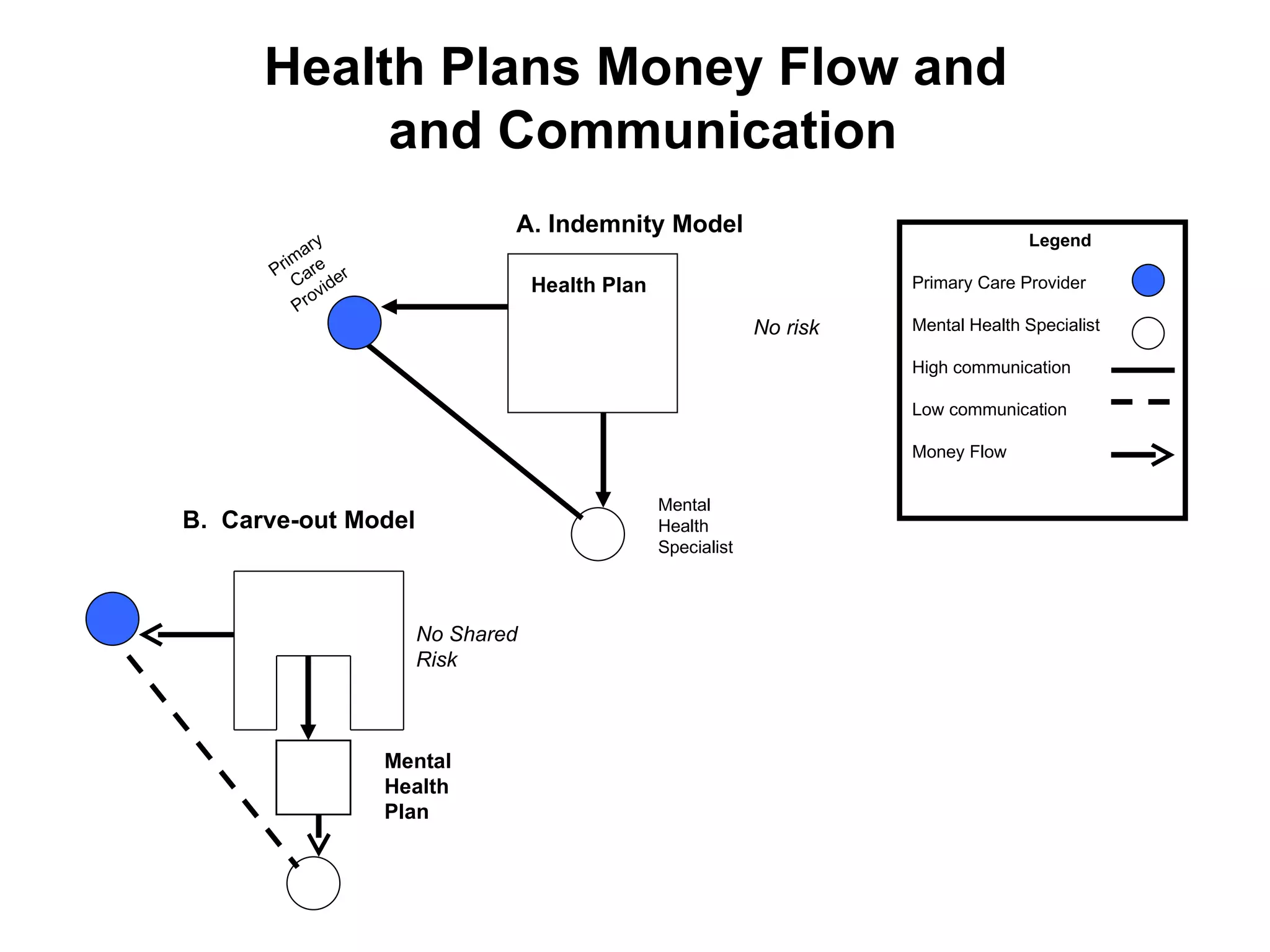
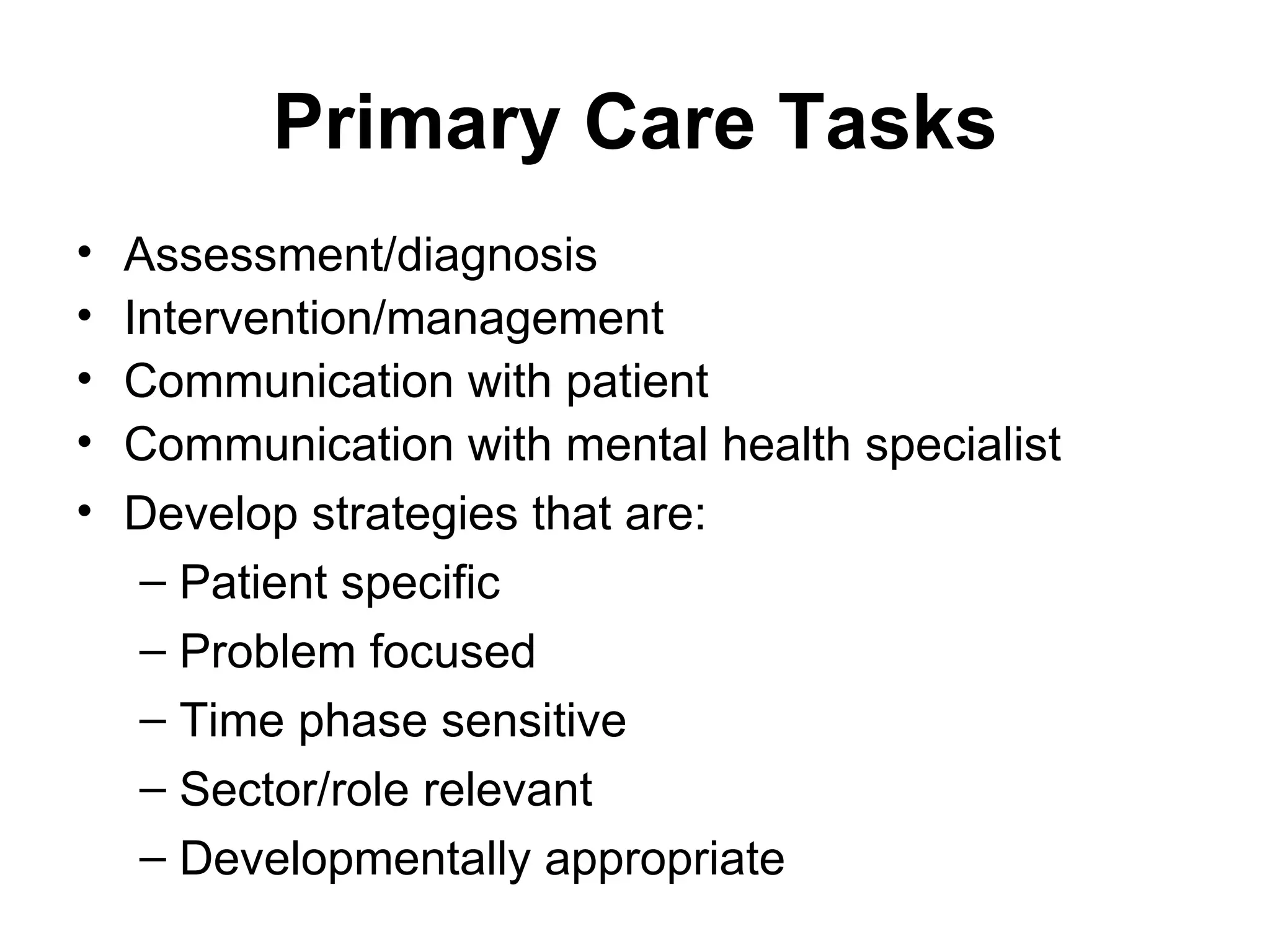
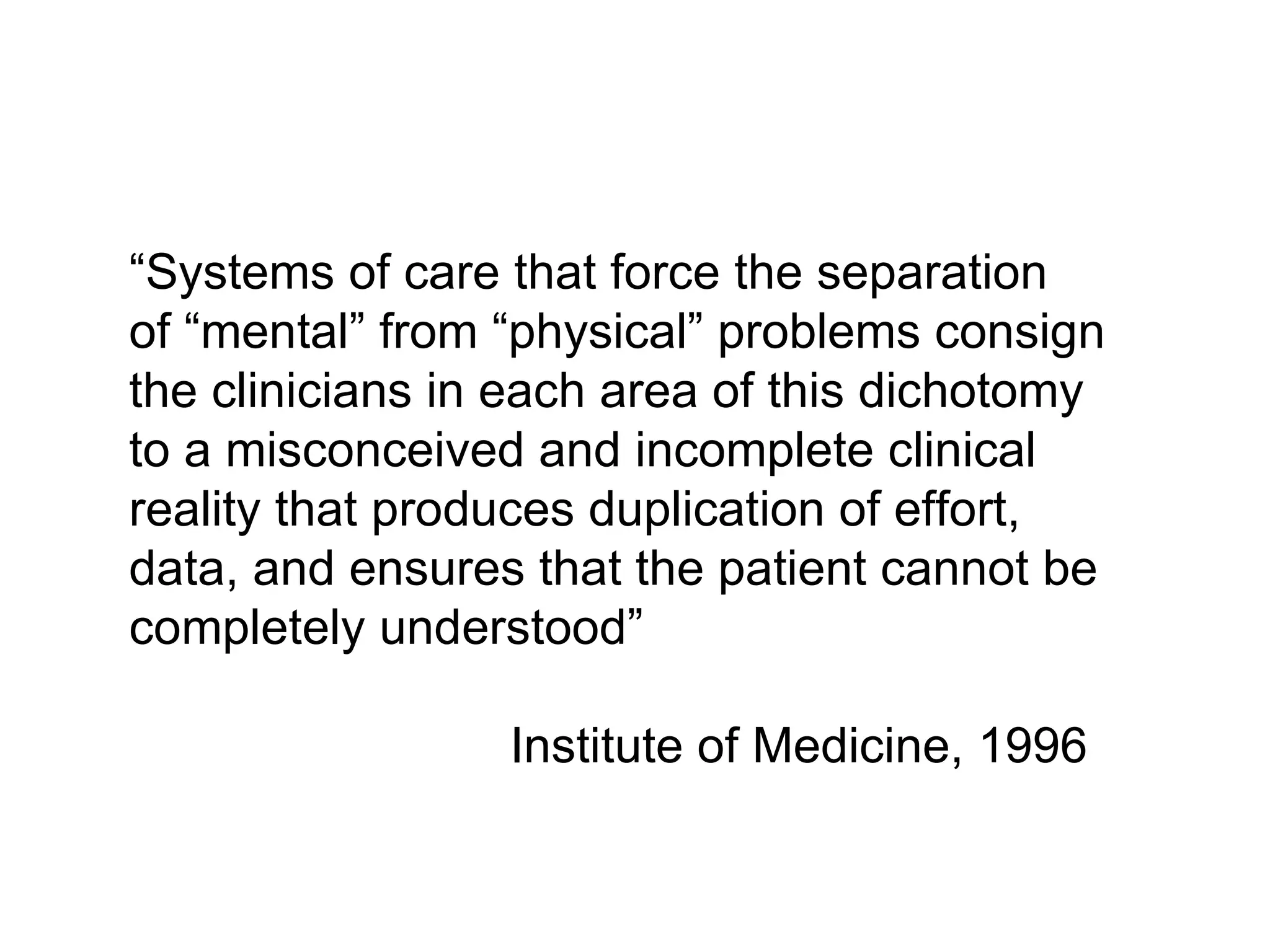
The document discusses barriers to integrating behavioral health and primary care. Some key barriers include different conceptual models between primary care and specialty mental health care, lack of provider time and training, and organizational and financial barriers between practices. Steps to improve care include adopting a problem-focused approach in primary care, clarifying roles and responsibilities between primary care physicians and behavioral health specialists, and facilitating better communication and coordination between providers.