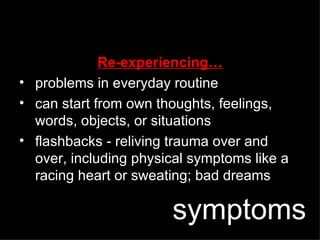
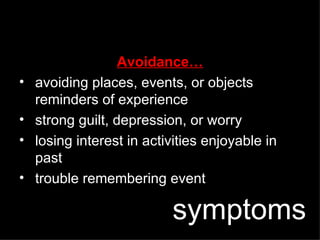
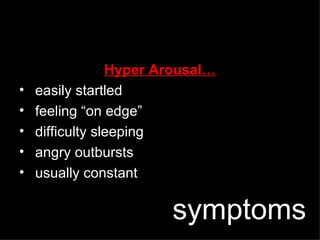
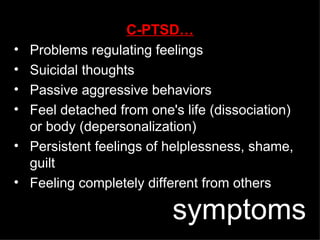
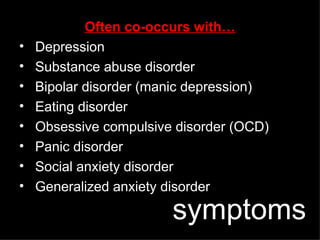
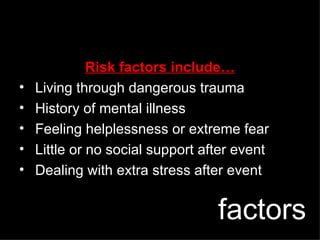
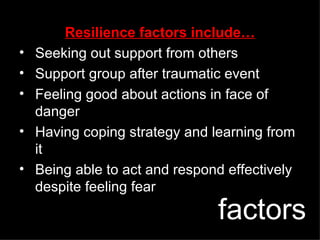
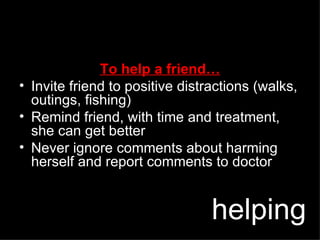
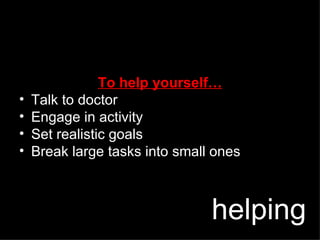
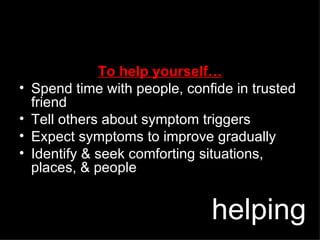
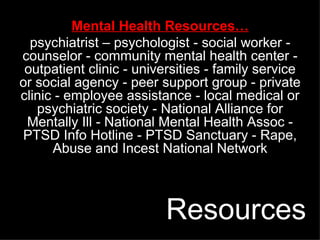
PTSD, also known as "soldier's heart," is an anxiety disorder that can develop after exposure to a terrifying event where serious physical harm was threatened. In PTSD, the normal fear response remains activated even when no longer in danger. Symptoms include re-experiencing the traumatic event through thoughts and flashbacks, avoiding reminders, and feeling in a constant state of hyperarousal. Complex PTSD involves prolonged trauma exposure and long-term problems with emotions and social functioning. Treatment involves psychotherapy like exposure therapy and cognitive restructuring, as well as medication in some cases. Social support from family and friends is also important for treatment.