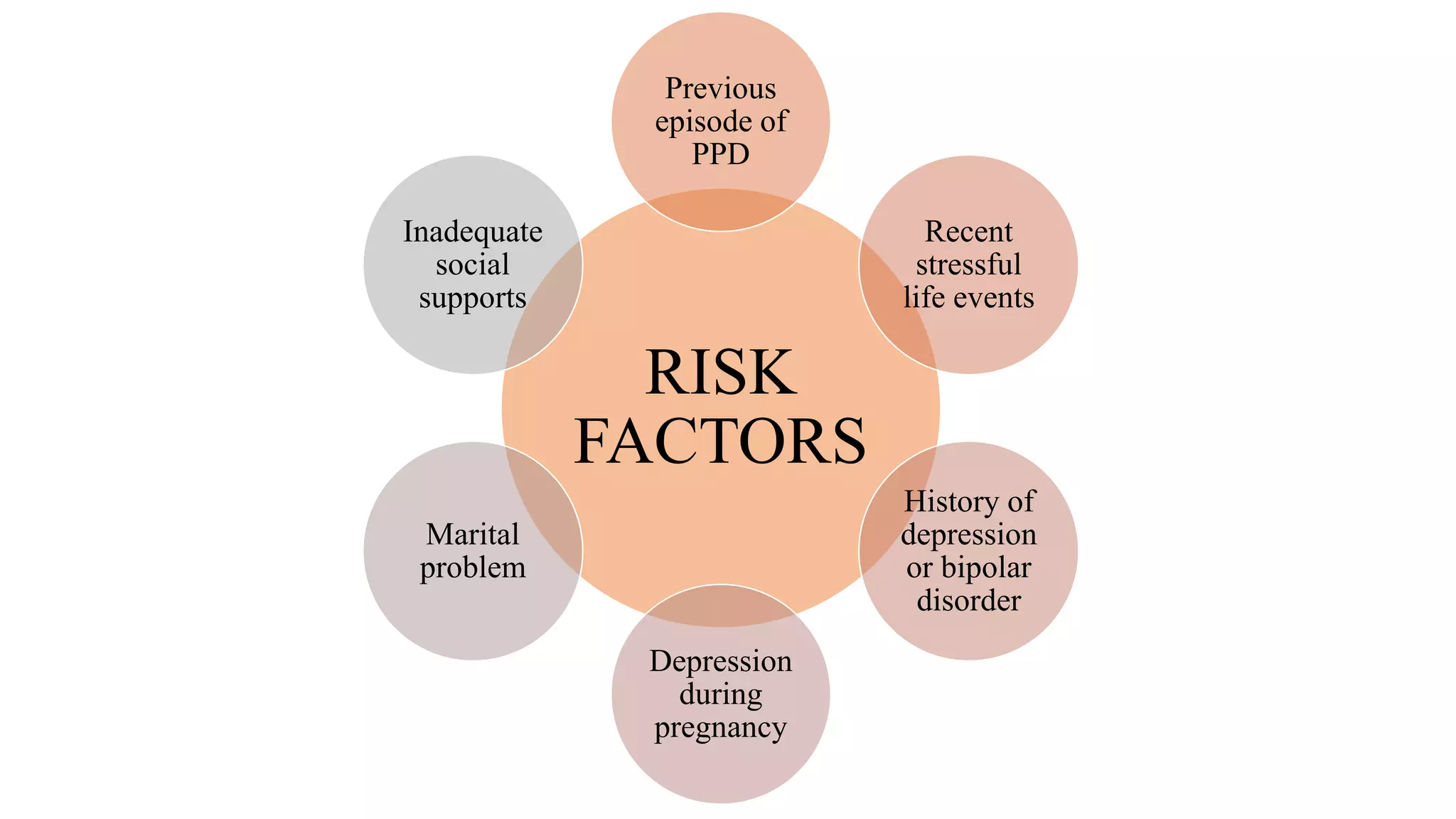
The document discusses postpartum psychiatric disorders, highlighting the prevalence and risk factors of conditions such as postpartum blues, postpartum depression (PPD), and postpartum psychosis. Approximately 85% of women experience some mood disturbance during the postpartum period, with 10-15% developing significant symptoms of depression or anxiety, while postpartum psychosis is rare but severe, necessitating immediate medical intervention. Treatment options vary from psychosocial support for postpartum blues to pharmacological options for PPD and urgent care for postpartum psychosis.







































![REFERENCES
Batt MM, Duffy KA, Novick AM, Metcalf CA, Epperson CN. Is Postpartum Depression Different From
Depression Occurring Outside of the Perinatal Period? A Review of the Evidence. Focus (Am Psychiatr
Publ). 2020;18(2):106-119. doi:10.1176/appi.focus.20190045
Balaram K, Marwaha R. Postpartum Blues. [Updated 2022 Feb 7]. In: StatPearls [Internet]. Treasure Island
(FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554546/
Gavin NI, Gaynes BN, Lohr KN, et al. : Perinatal depression: a systematic review of prevalence and
incidence. Obstet Gynecol 2005; 106:1071–1083 10.1097/01.AOG.0000183597.31630.db
MacQueen GM, Frey BN, Ismail Z, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT)
2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 6. Special
Populations: Youth, Women, and the Elderly. The Canadian Journal of Psychiatry. 2016;61(9):588-603.
doi:10.1177/070674371665927](https://image.slidesharecdn.com/postpartumpsychiatricdisorders-220426051159/75/POSTPARTUM-PSYCHIATRIC-DISORDERS-pptx-46-2048.jpg)
![Mesut Işık. Postpartum Psychosis. Eastern J Med. 2018; 23(1): 60-63
Milgrom J, Gemmill AW, Ericksen J, et al. : Treatment of postnatal depression with cognitive behavioural
therapy, sertraline and combination therapy: a randomised controlled trial. Aust N Z J
Psychiatry 2015; 49:236–245 10.1177/0004867414565474
Perry A, Gordon-Smith K, Jones L, Jones I. Phenomenology, Epidemiology and Aetiology of Postpartum
Psychosis: A Review. Brain Sciences. 2021; 11(1):47. https://doi.org/10.3390/brainsci11010047
Protheroe C. Puerperal psychosis: A long-term study 1927–1961. Br J
Psychiatry. 1969;111:9. [PubMed] [Google Scholar]
Van Niel MS, Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May;87(5):273-277. doi:
10.3949/ccjm.87a.19054. PMID: 32357982
Wisner KL, Moses-Kolko EL, Sit DKY: Postpartum depression: a disorder in search of a definition. Arch
Women Ment Health 2010; 13:37–40 10.1007/s00737-009-0119-9](https://image.slidesharecdn.com/postpartumpsychiatricdisorders-220426051159/75/POSTPARTUM-PSYCHIATRIC-DISORDERS-pptx-47-2048.jpg)
