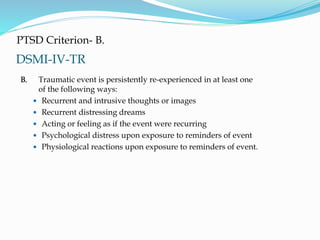
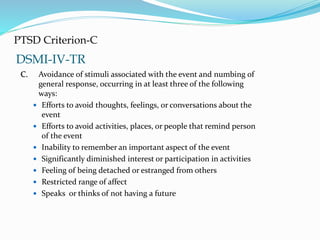
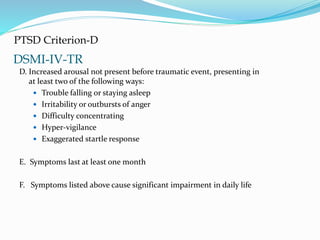
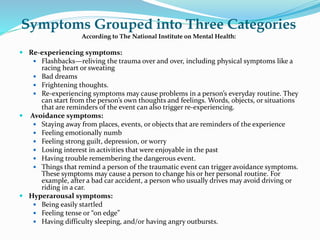
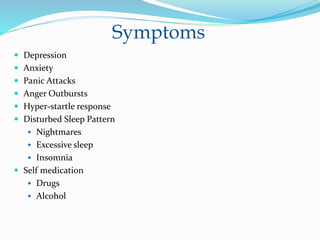
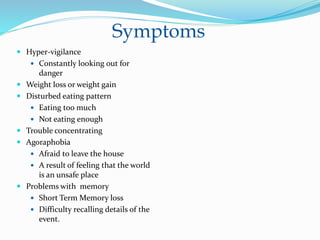
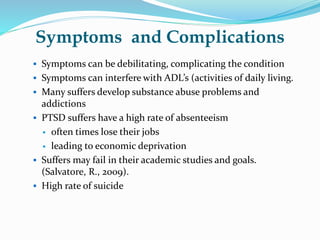
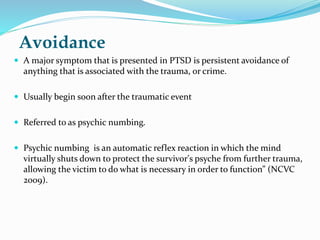
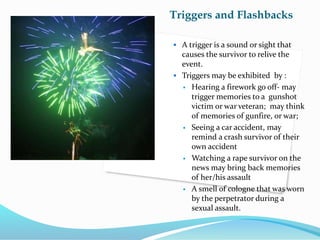
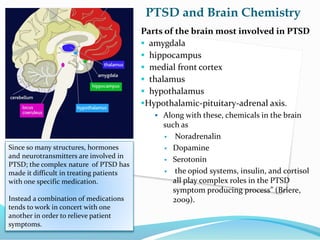
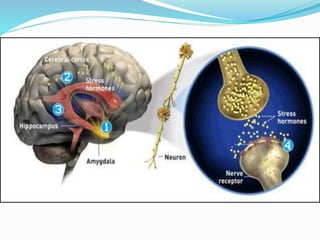
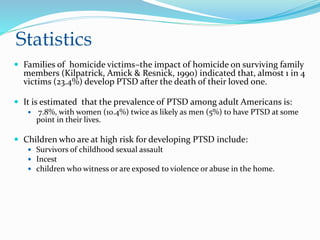
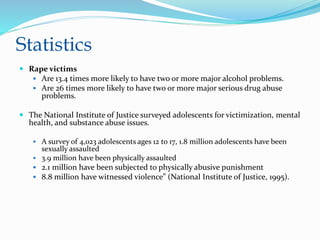
The document outlines the nature, symptoms, and treatment of post-traumatic stress disorder (PTSD), emphasizing its impact beyond just veterans to include crime victims and various traumatic events. It discusses PTSD's prevalence, particularly among vulnerable populations like children and survivors of violence, along with its psychological consequences and complex connections to brain chemistry. Treatment options such as therapy, medication, and Eye Movement Desensitization and Reprocessing (EMDR) are highlighted as essential for recovery.