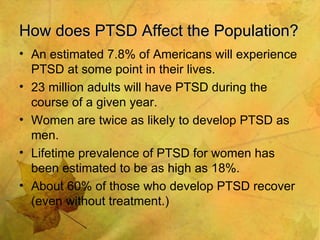
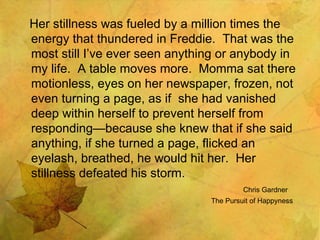
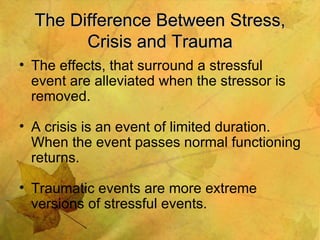
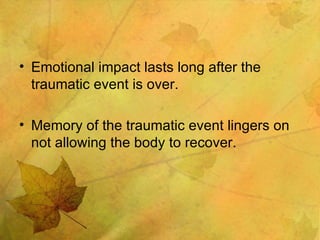
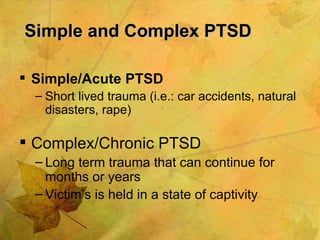
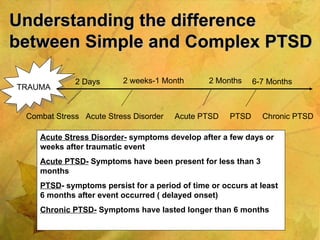
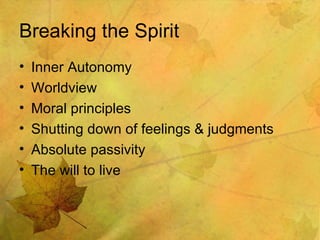
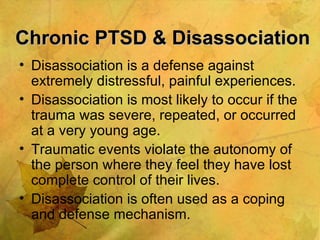
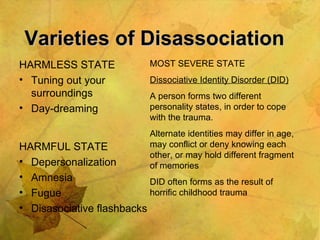
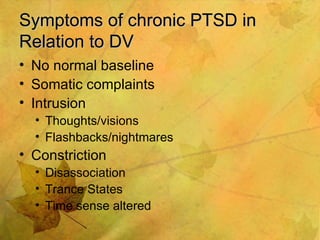
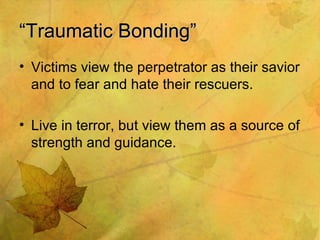
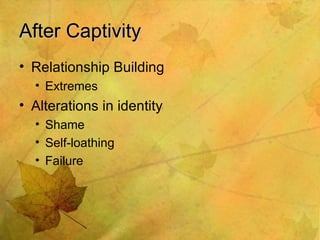
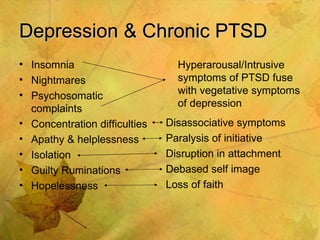
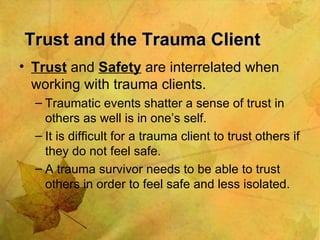
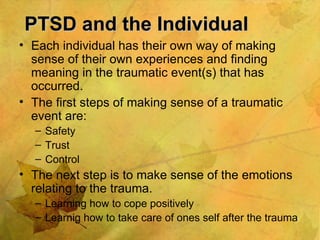
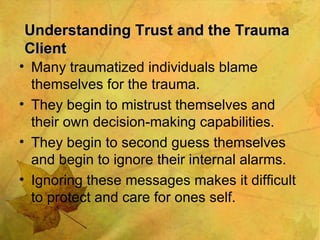
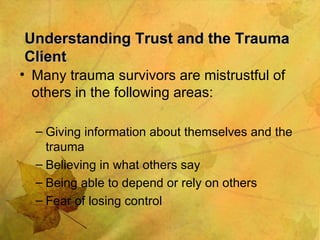
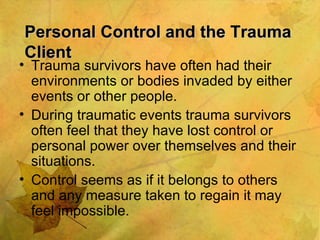
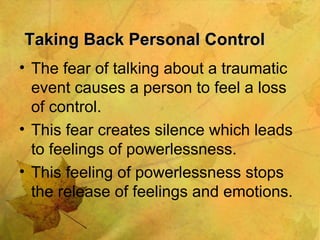
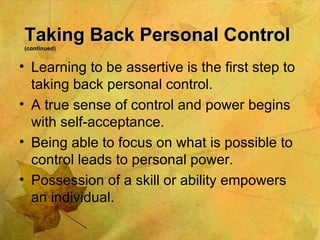
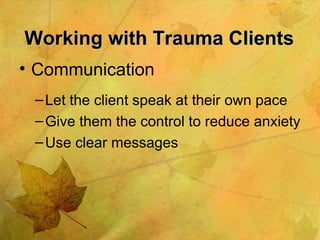
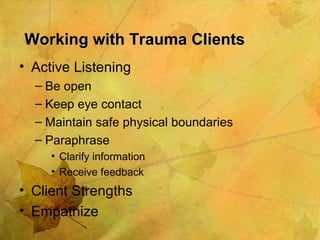
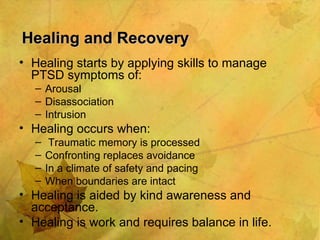
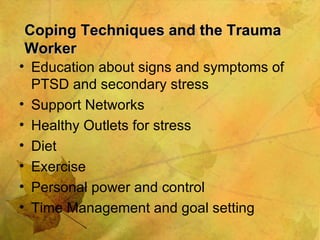
The document discusses post-traumatic stress disorder (PTSD) and its relationship to domestic violence. It defines PTSD and explains that it is more likely to be chronic or complex form when the trauma involves prolonged domestic violence. Symptoms of chronic PTSD include dissociation, intrusive thoughts, and loss of control. The document also discusses how trauma impacts trust and control, and strategies for healing and reducing secondary trauma for support workers.