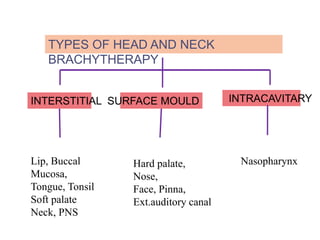
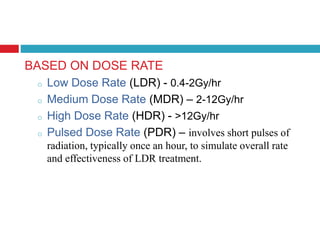
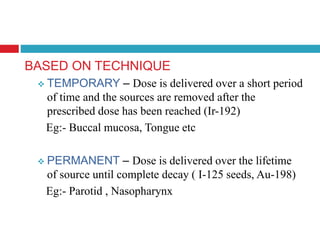
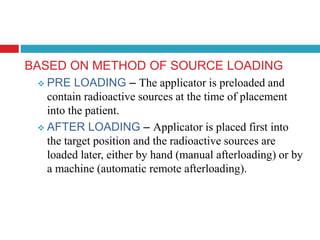
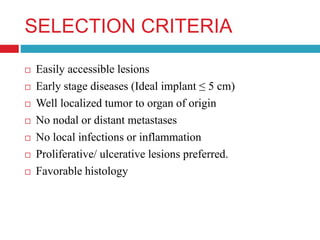
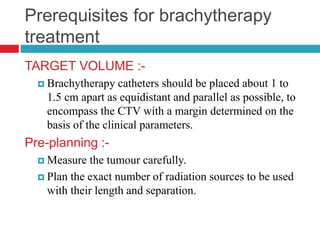
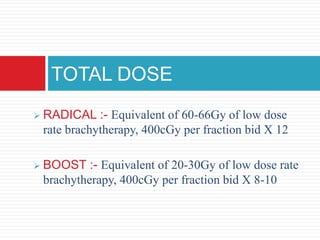
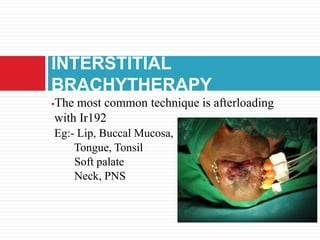
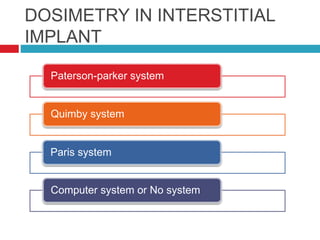
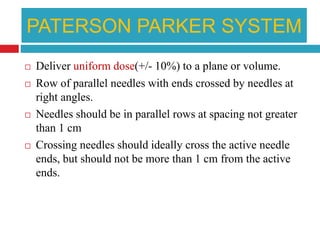
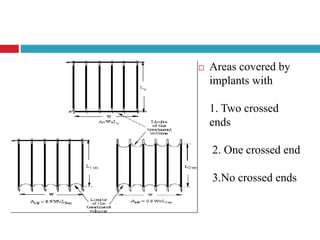
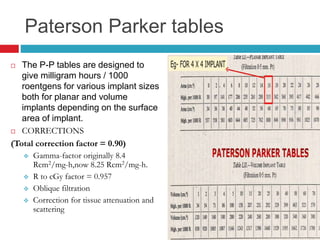
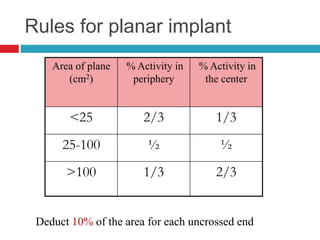
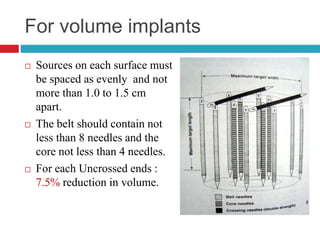
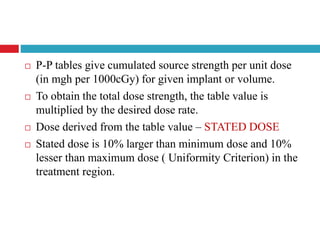
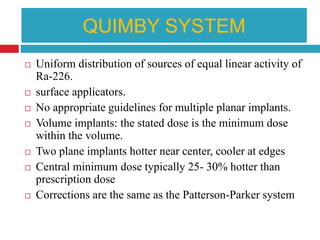
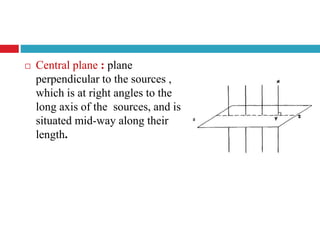
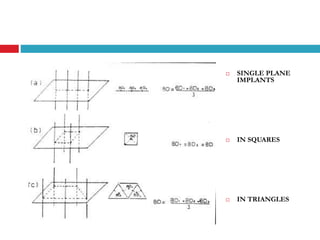
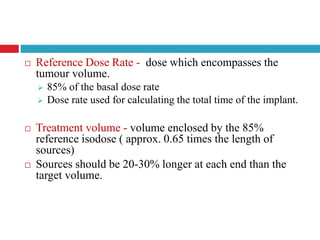
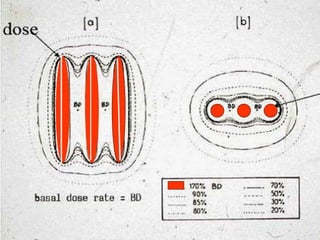
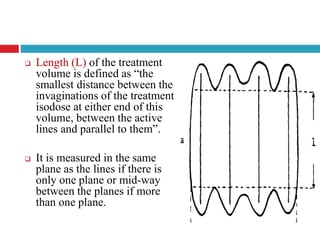
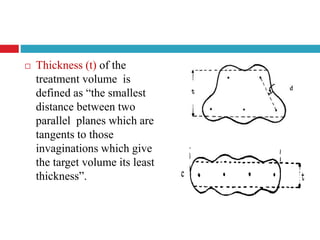
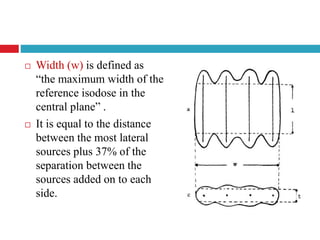
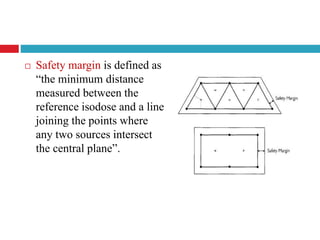
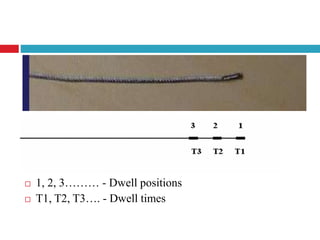
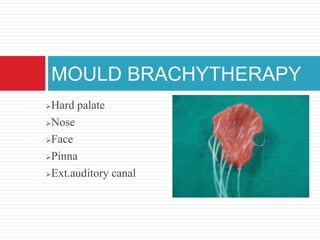
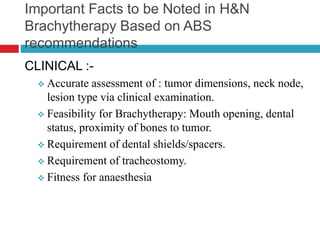
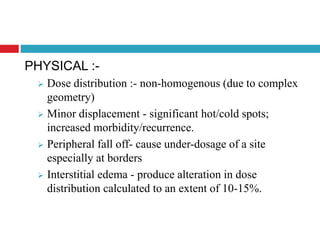
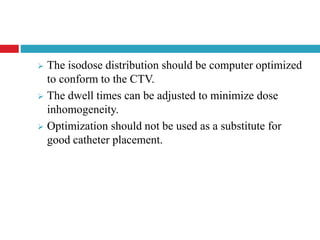
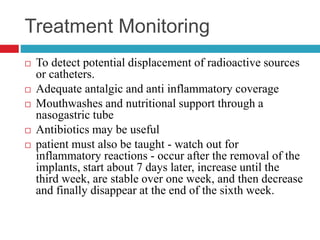
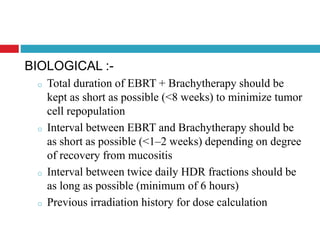
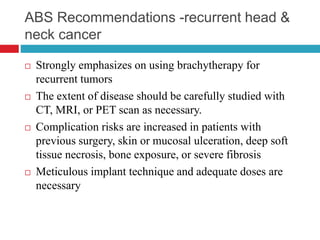
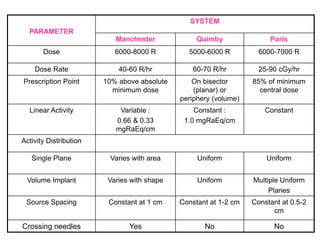
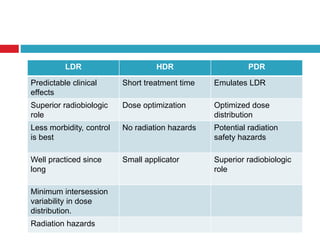
This document discusses brachytherapy techniques for head and neck cancers. It describes different types of brachytherapy based on positioning of the radionuclide (interstitial, intracavitary, surface moulds), dose rate (LDR, MDR, HDR, PDR), and technique (temporary, permanent). It also discusses dosimetry systems like Patterson-Parker, Quimby, Paris and computerized planning. Key aspects of treatment planning, delivery, and post-treatment care are summarized. Advantages include localized high dose with rapid falloff and organ preservation, while limitations include inaccessibility and quality dependence on implant. American Brachytherapy Society guidelines emphasize accurate assessment and dental