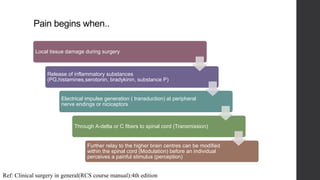
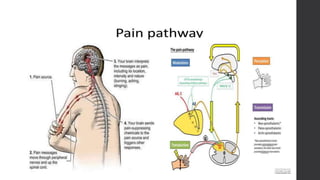
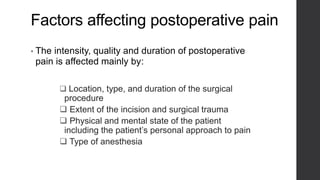
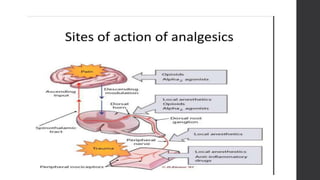
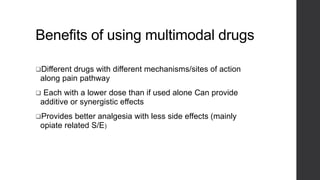
Postoperative pain management is an essential component of surgical patient care. About 75% of surgical patients experience pain after a procedure. Effective pain control allows for early mobilization, reduced complications, and faster recovery. Postoperative pain arises from tissue damage during surgery and the subsequent inflammatory response. Both pharmacological and non-pharmacological methods can be used to treat postoperative pain, including opioids, NSAIDs, local anesthetics, and physical therapy. Proper assessment and an individualized treatment plan that utilizes a stepwise multimodal approach can provide pain relief and optimize patient outcomes.