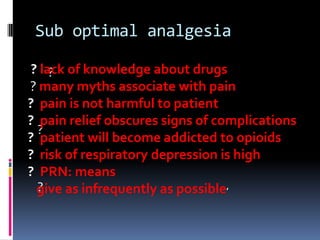
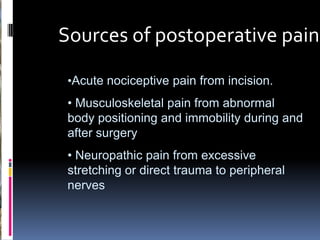
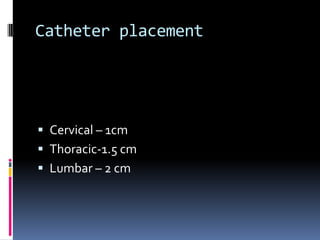
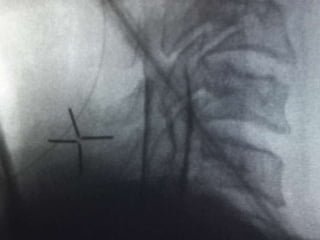
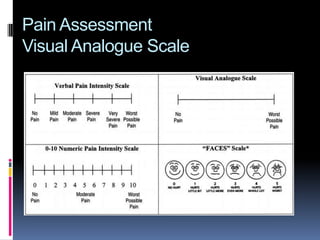
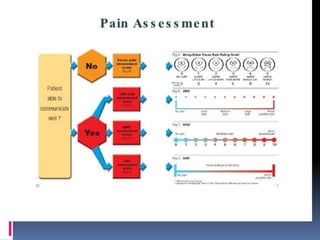
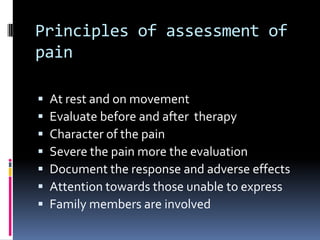
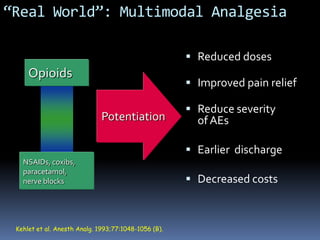
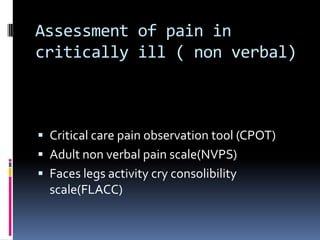
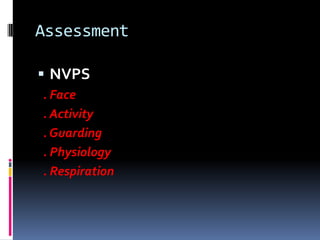
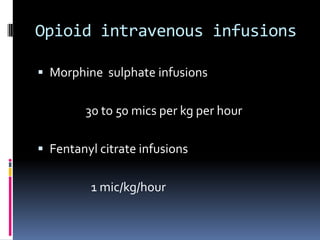
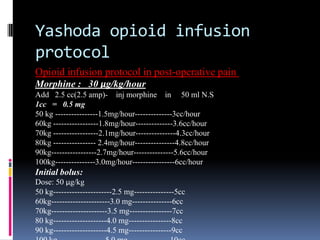
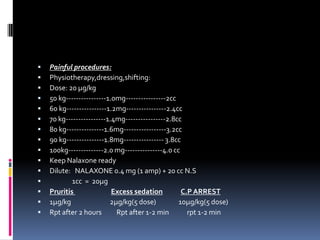
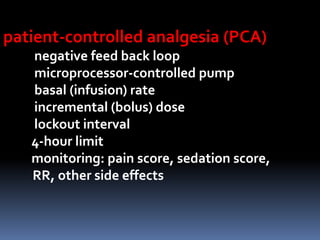
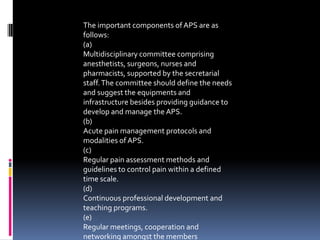
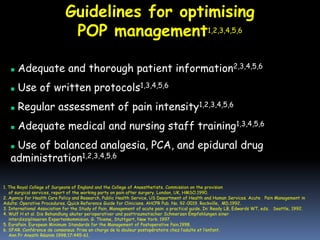
Dr. Sudheer Dara is a consultant anesthesiologist and pain specialist at Yashoda Hospital Secunderabad. He is the honorary treasurer of ISSP AP Chapter and founder of YAPM. His special interests include interventional pain management, ultrasound regional anesthesia, postoperative pain, acute pain services, and oral and injectable drugs. He discusses the need for improved postoperative pain management, highlighting issues like suboptimal analgesia, myths about pain relief, and inadequate assessment. He emphasizes the importance of multimodal analgesia using combinations of opioids, NSAIDs, paracetamol, nerve blocks, and the need for acute pain services with protocols and staff training to optimize postoperative pain management.