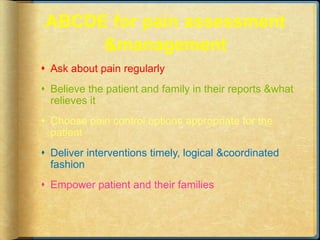
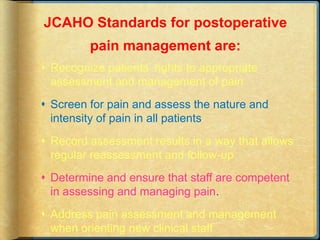
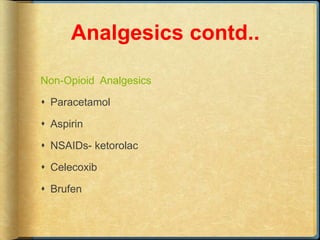
This document discusses pain, including definitions of pain, types of pain, factors influencing pain, effects of pain, individual variations in pain response, and pain assessment tools. It also covers postoperative pain management principles like the WHO pain ladder, pharmacological and non-pharmacological interventions for pain control, preemptive analgesia using local anesthetics or other drugs before a painful stimulus to reduce later pain, and techniques like patient-controlled analgesia and epidural analgesia. The goal of pain management is to prevent pain from interfering with recovery through adequate assessment and treatment.