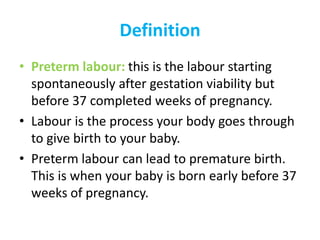
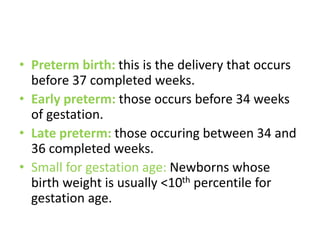
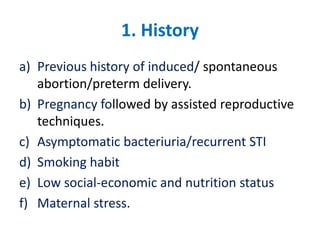
Preterm labour can occur before 37 weeks of pregnancy and lead to premature birth. It has multiple potential causes including prior preterm delivery, infections, medical complications in the present pregnancy, cervical issues, or no known cause. Diagnosis involves examining the cervix and checking for contractions. Management focuses on preventing preterm labour if possible through risk factor identification and interventions like bed rest. If it cannot be prevented, care involves arresting labour and providing effective neonatal support for underdeveloped babies.