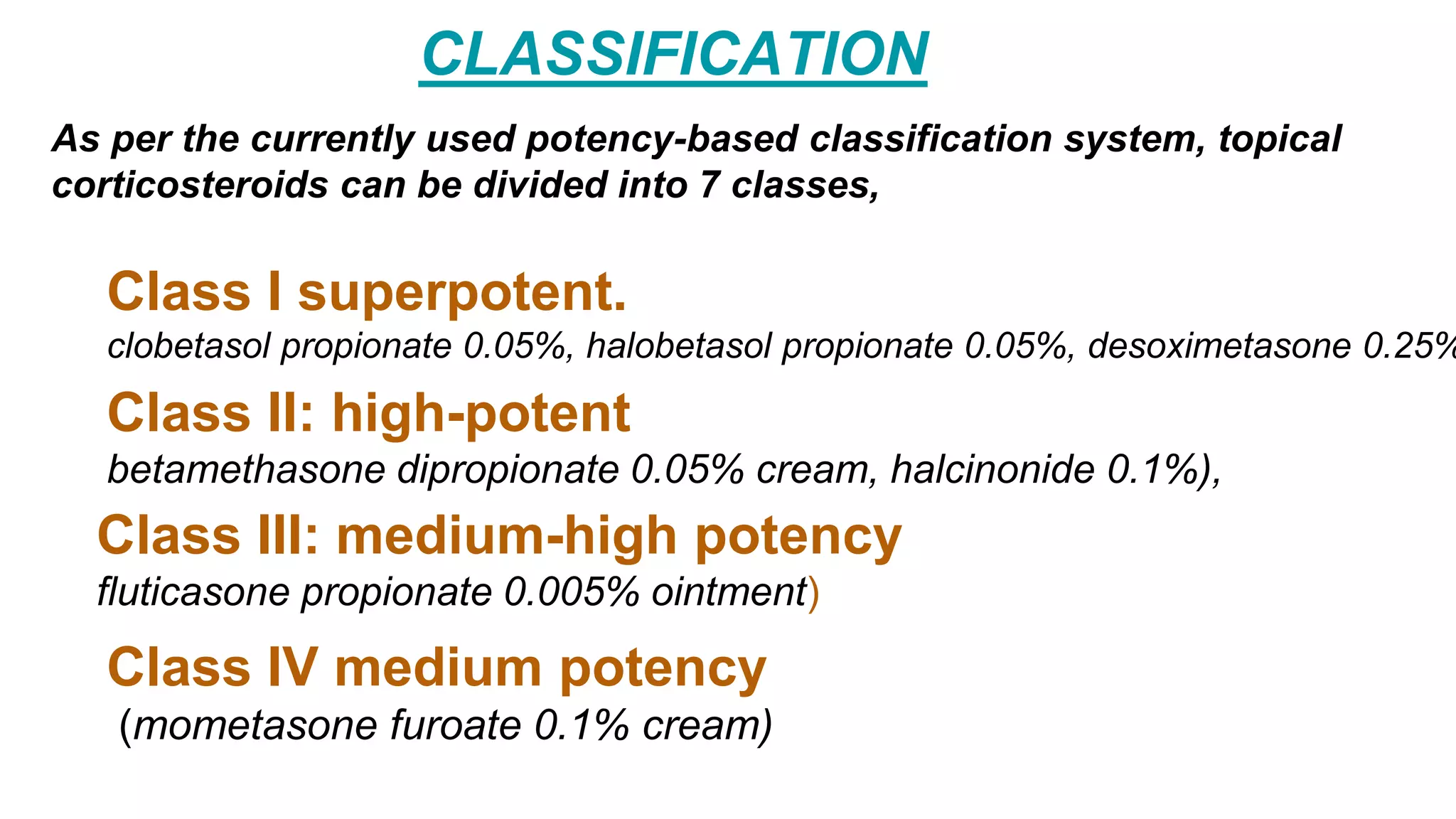
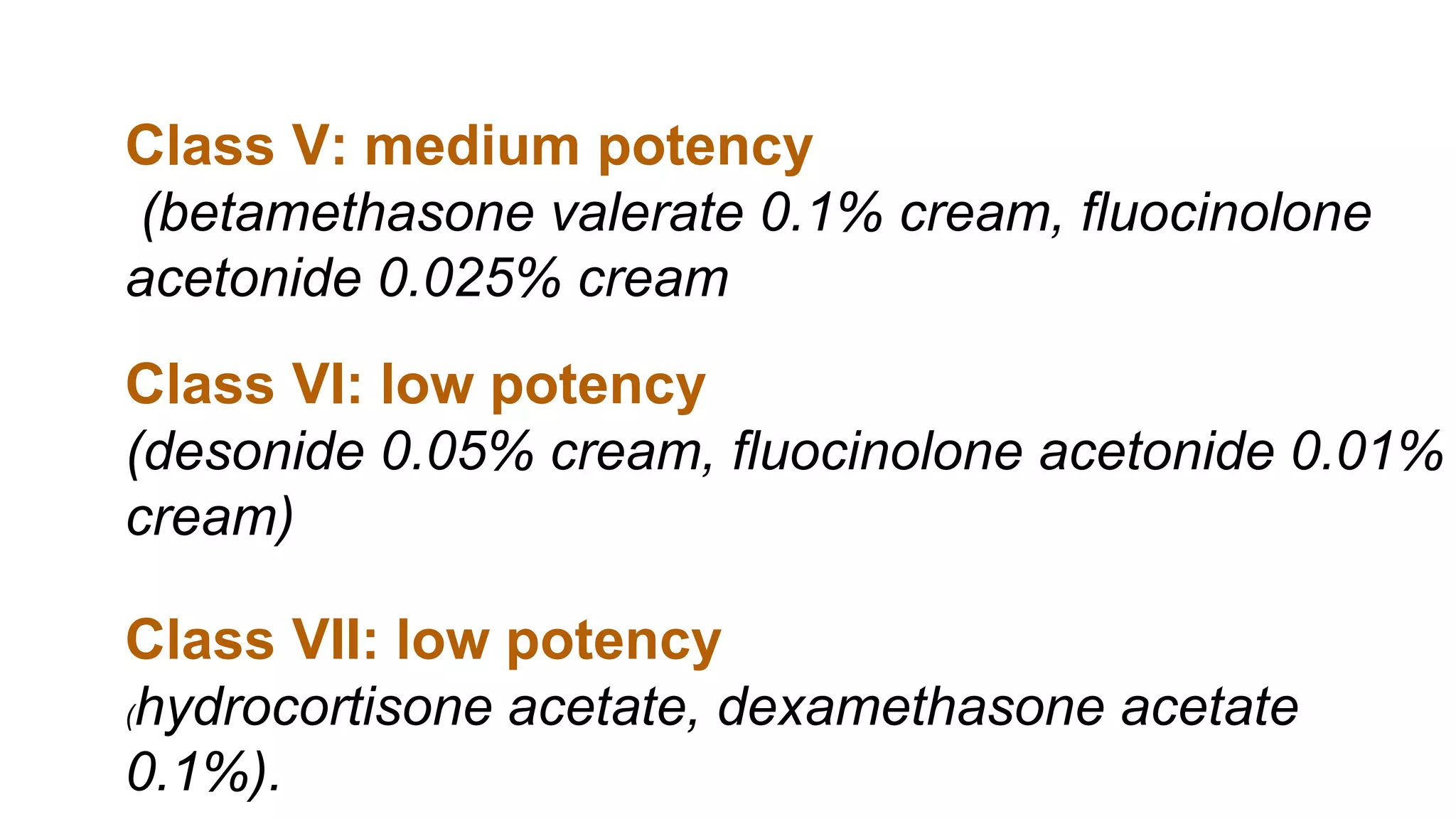
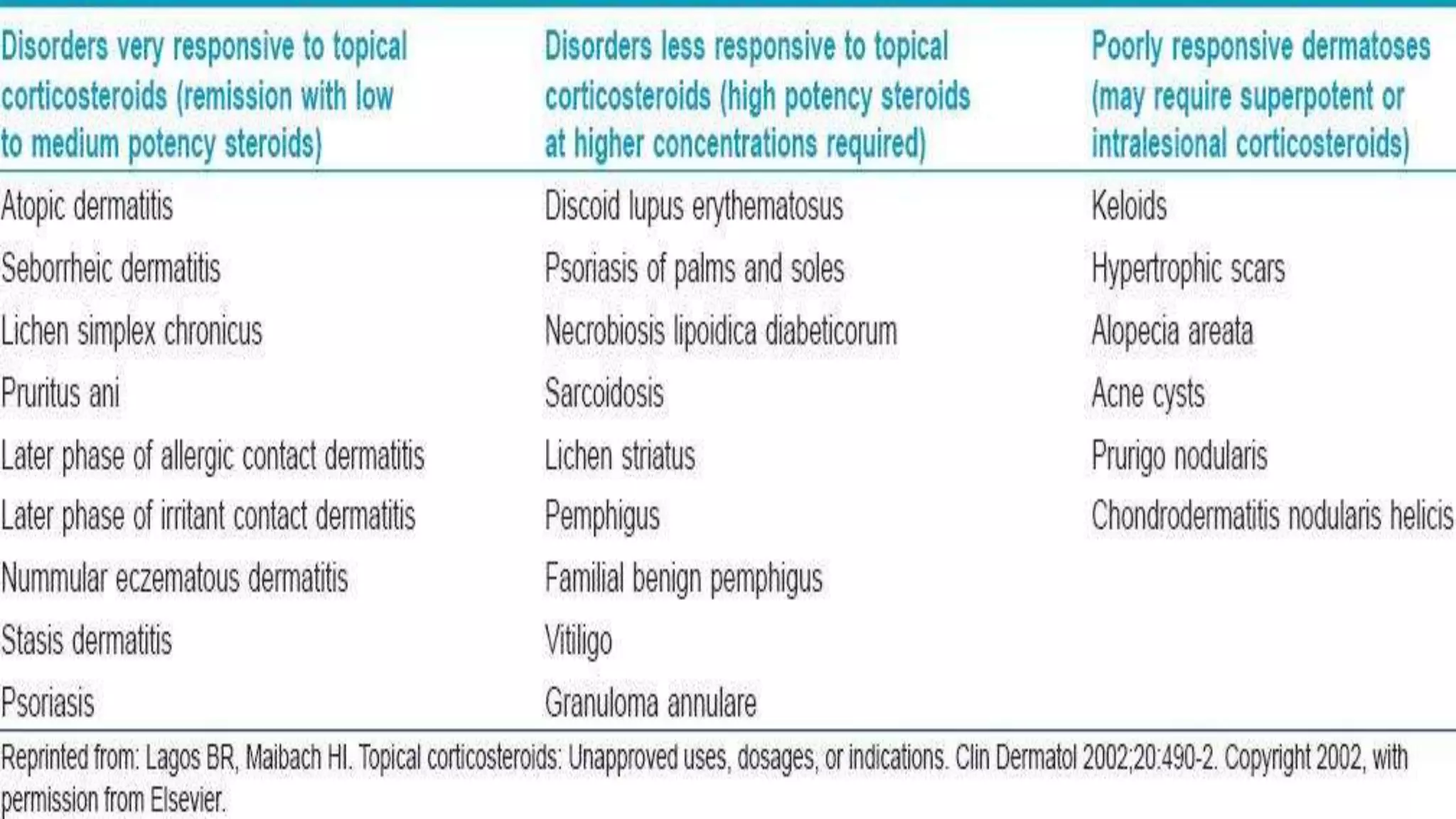
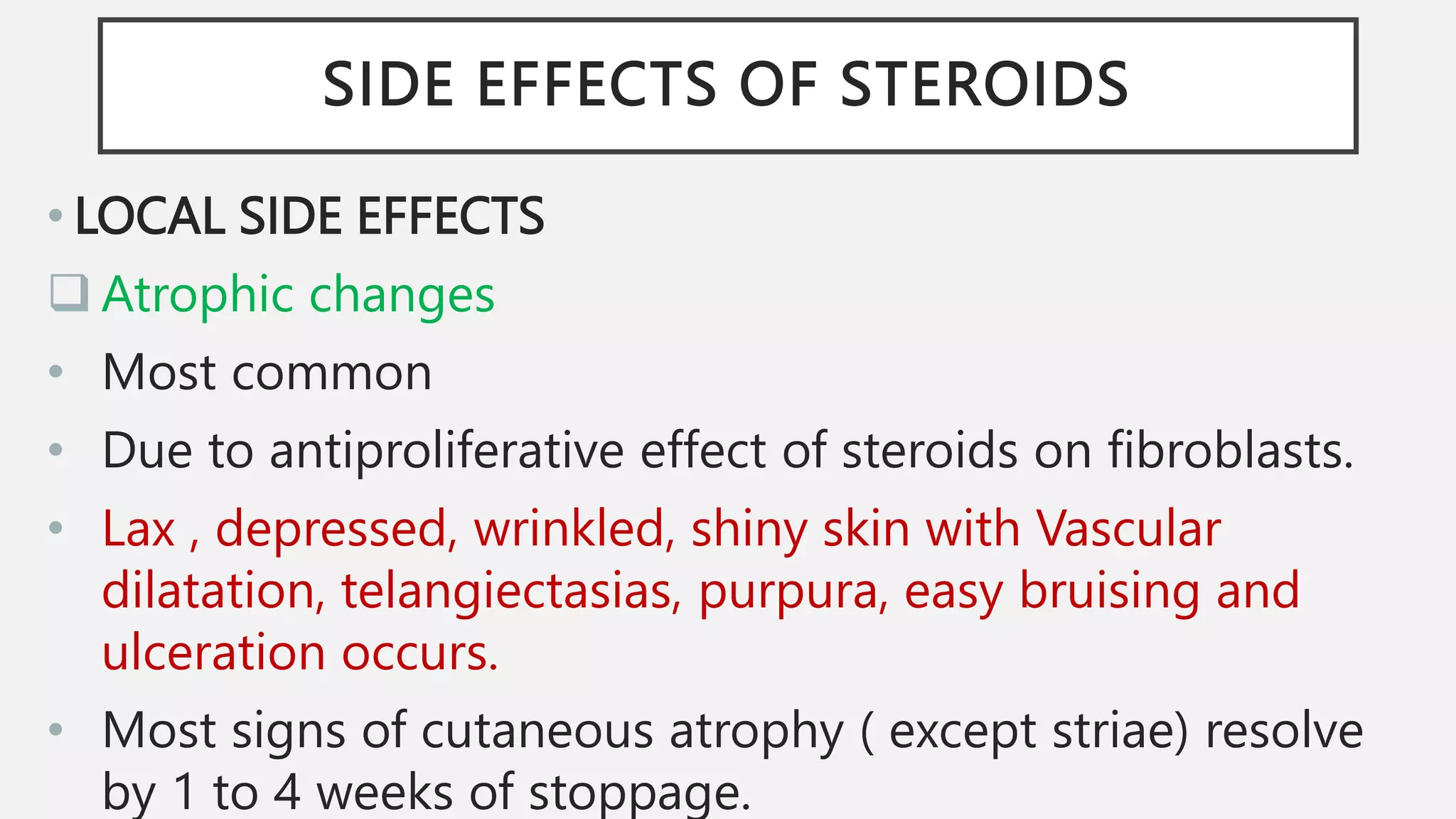
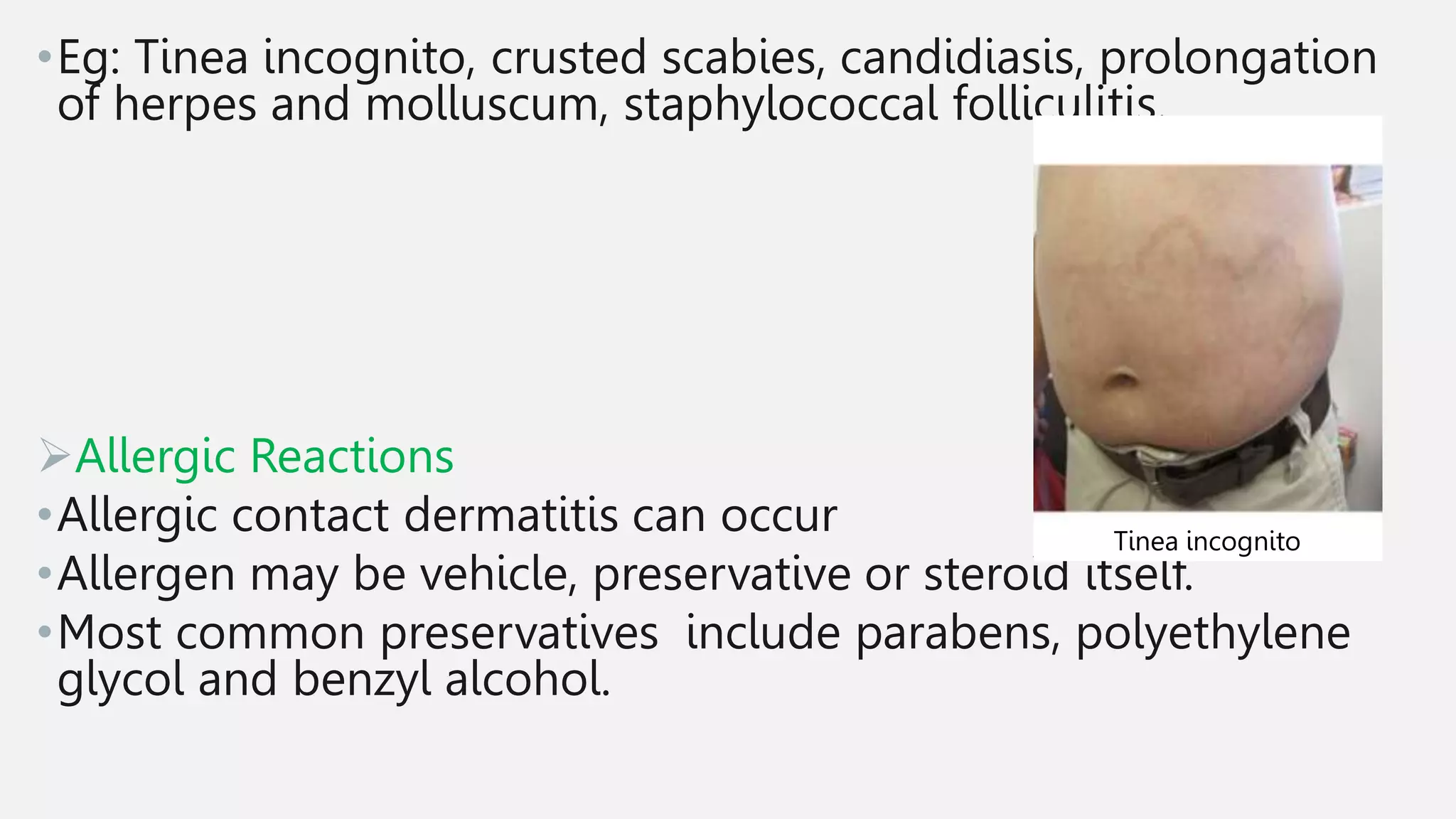
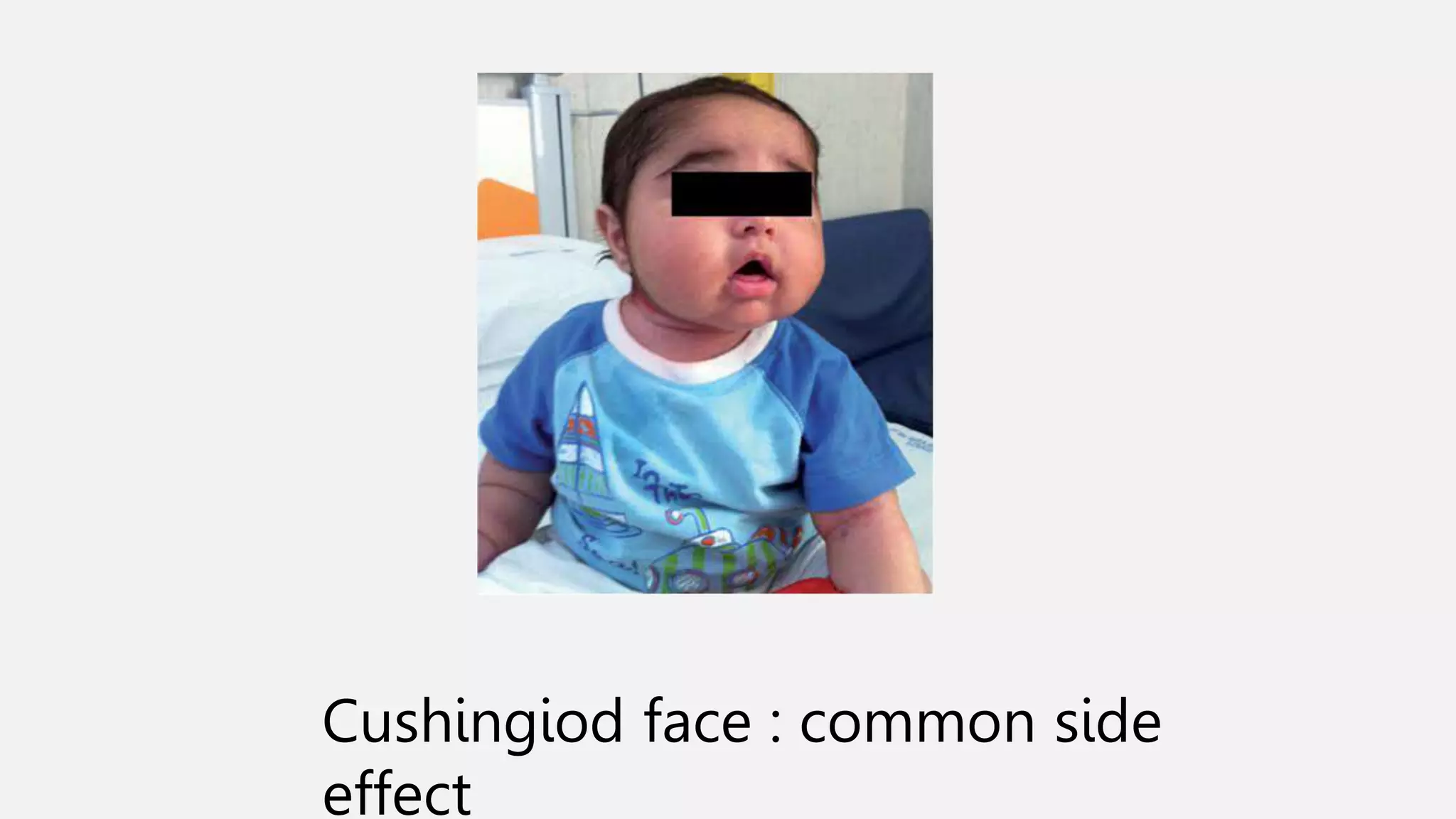
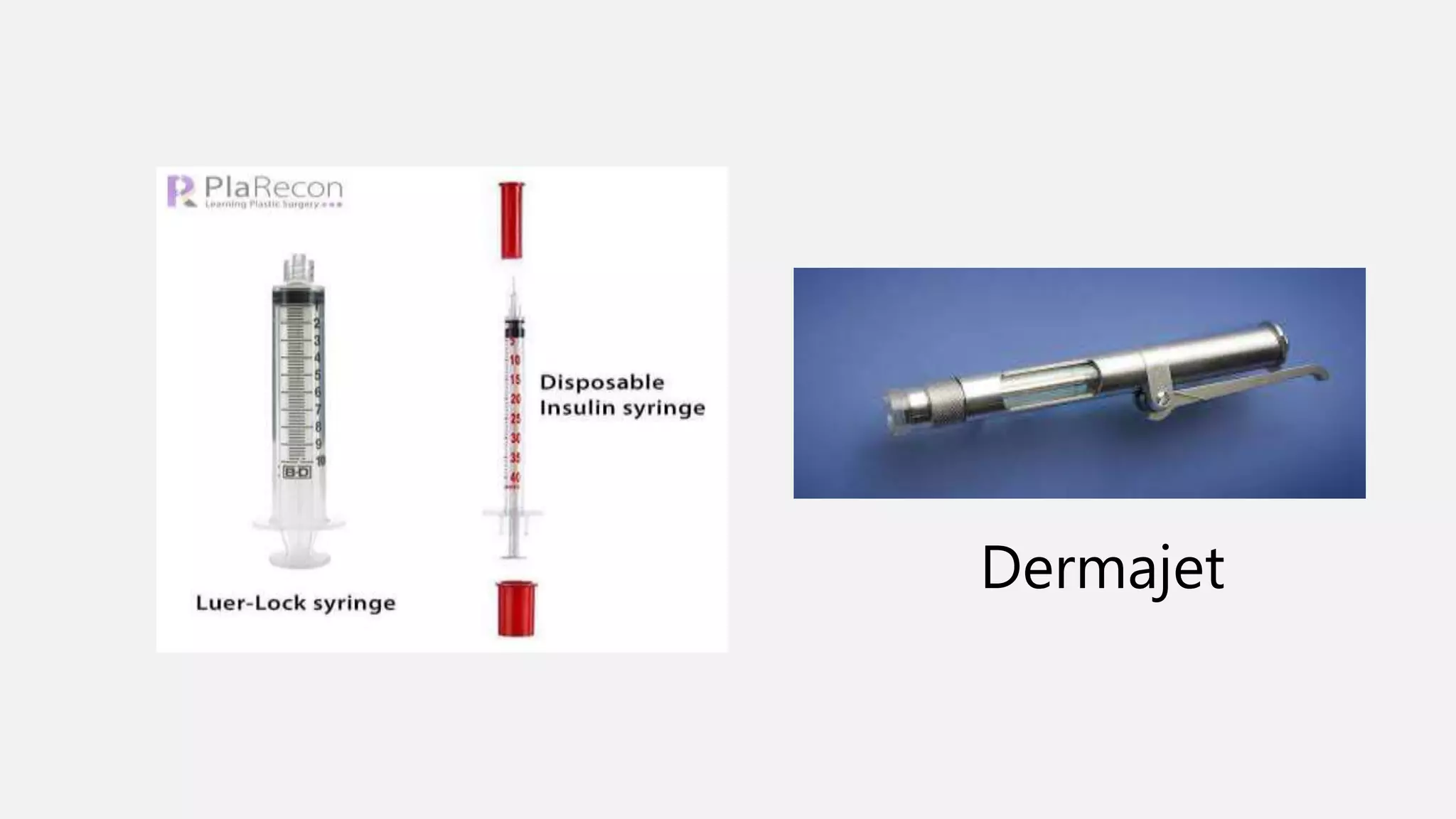
Corticosteroids can be divided into 7 classes based on potency. Topical corticosteroids are used to treat inflammatory skin conditions and their potency depends on the condition. Potential local side effects include atrophy, acneiform reactions, and infections. Systemic side effects may include HPA axis suppression, diabetes, and growth retardation in children. Intralesional steroid injections bypass the skin barrier for better delivery and less atrophy. Conditions treated include alopecia areata, keloids, and resistant psoriasis.