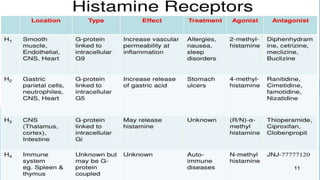
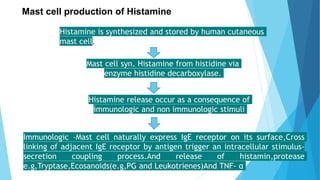
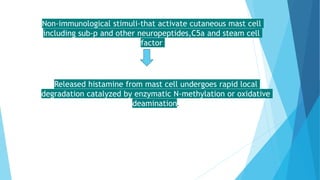
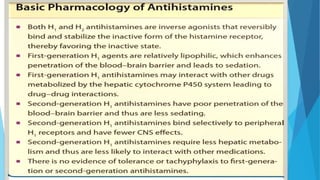
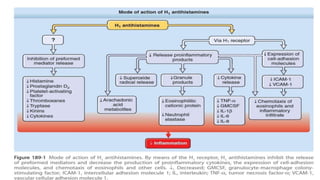
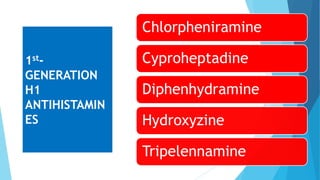
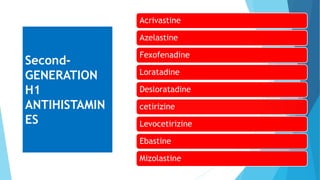
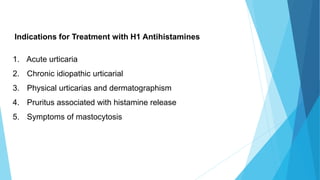
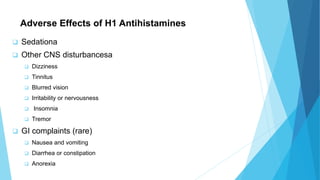
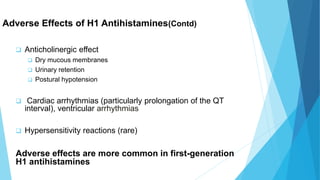
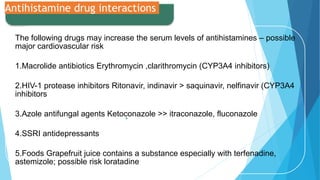
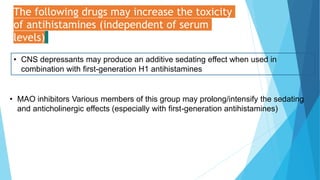
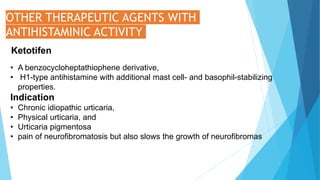
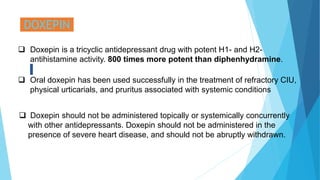
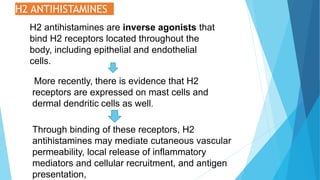
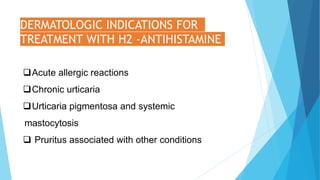
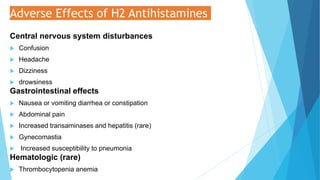
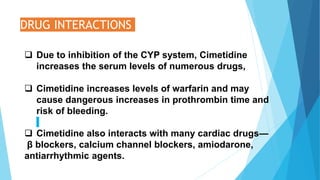
Antihistamines are used to treat conditions caused by the release of histamine such as allergic reactions and inflammation. There are first-generation and second-generation antihistamines that work by blocking the H1 and H2 receptors where histamine binds. First-generation antihistamines are more likely to cause sedation and anticholinergic side effects while second-generation antihistamines have fewer side effects. Antihistamines are used to treat acute and chronic urticaria, physical urticarias, pruritus, and symptoms of mastocytosis. Drug interactions and the risk of side effects must be considered when selecting an antihistamine, especially for special patient populations such as children, elderly