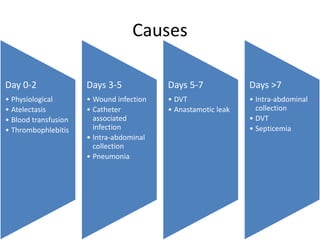
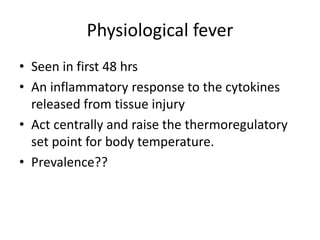
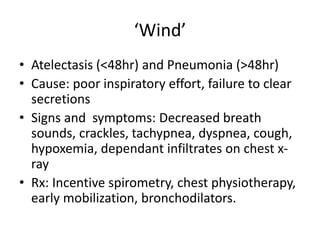
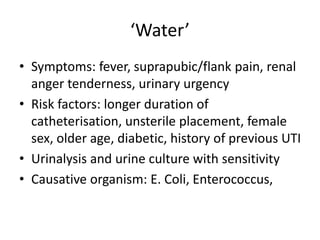
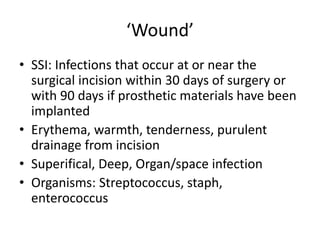
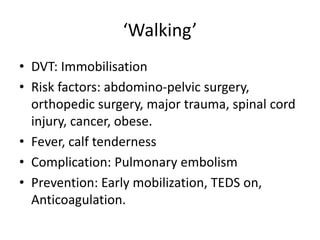
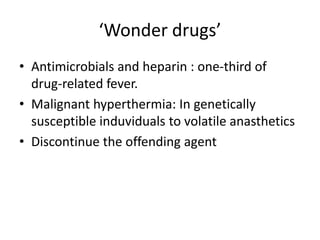
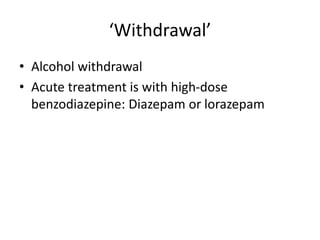
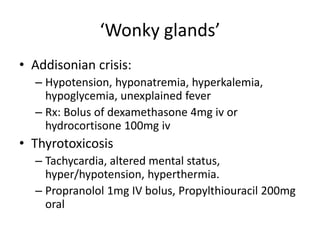
Postoperative fever can be caused by various physiological and infectious etiologies. Physiological fever occurring in the first 48 hours is a normal inflammatory response to tissue injury from surgery. Common causes of fever include atelectasis and pneumonia within the first 48 hours, and wound, urine, or intra-abdominal infections between days 3-7. Deep vein thrombosis is also a potential cause after days 5-7. A thorough evaluation including physical exam, lab tests, and imaging is needed to identify the source and guide appropriate treatment.