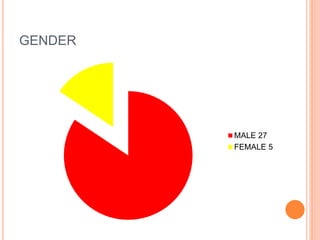
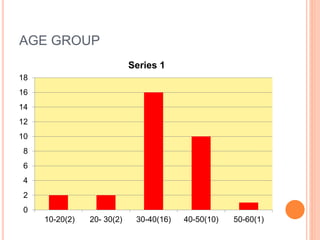
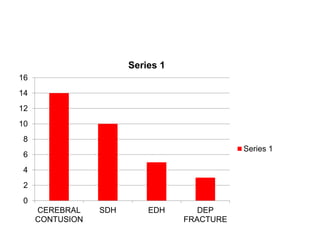
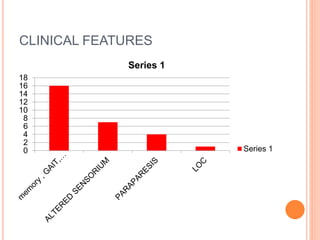
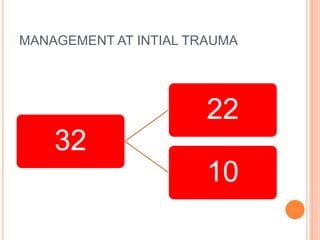
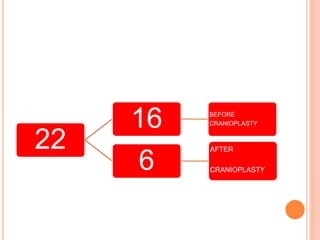
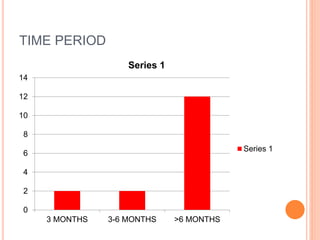
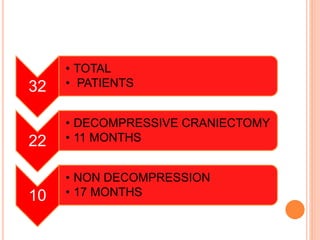
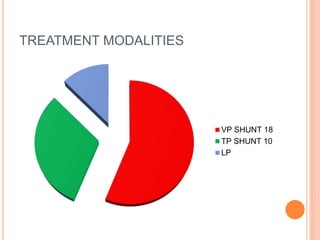
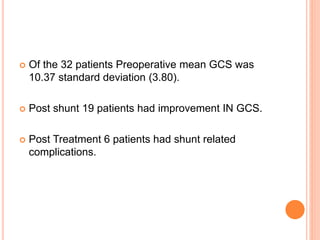
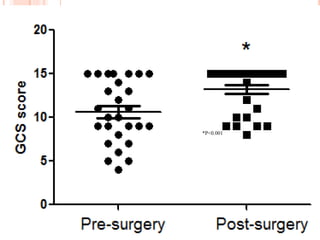
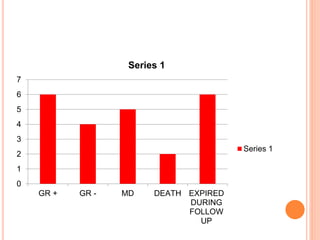
This document describes a case series study of 32 patients with post-traumatic hydrocephalus conducted at a hospital in Hyderabad, India between 2004-2016. The study aimed to examine the incidence, risk factors, prognosis factors, and Glasgow Outcome Scale for these patients. Key findings included that decompressive craniectomy and delays in bone flap replacement increased the risk of developing post-traumatic hydrocephalus. Clinical improvement was observed in most patients after ventricular-peritoneal shunt placement treatment.