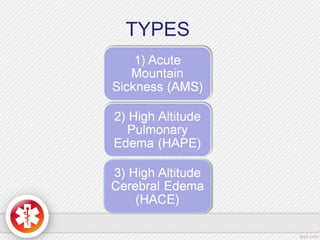
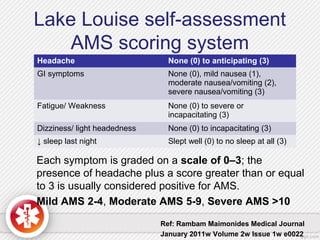
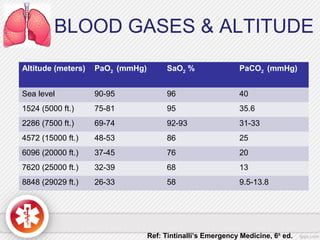
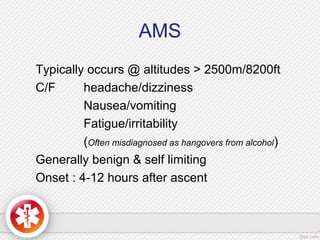
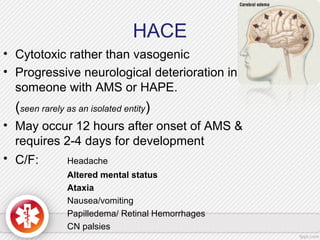
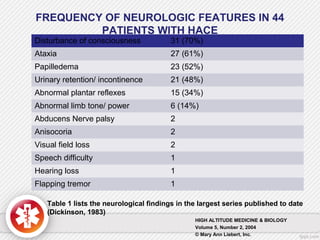
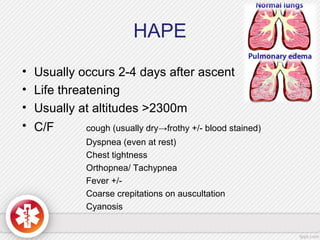
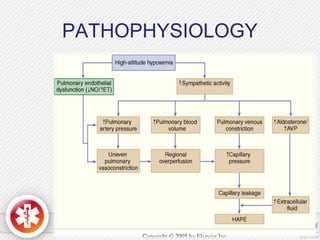
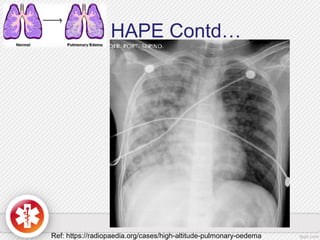
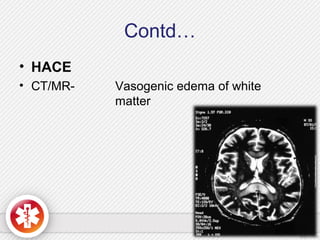
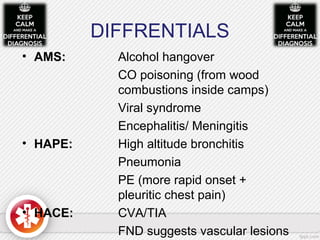
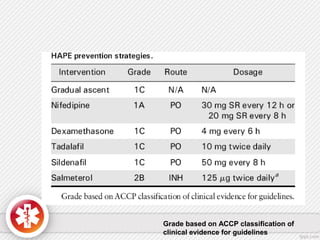
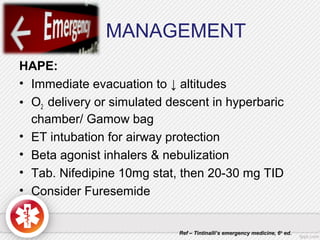
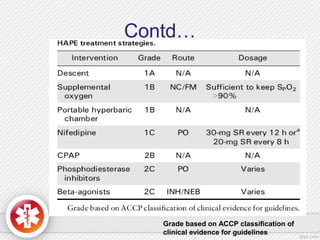
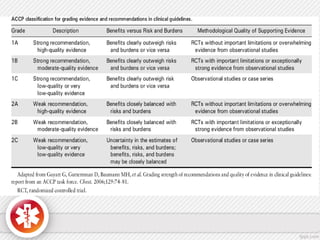
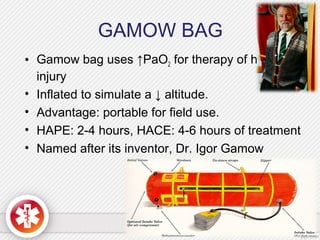
1) High altitude illness includes acute mountain sickness (AMS), high altitude cerebral edema (HACE), and high altitude pulmonary edema (HAPE). AMS causes headache, nausea, fatigue, and dizziness. HACE is a neurological deterioration in someone with AMS. HAPE causes cough, dyspnea, and chest tightness. (2) Risk factors for these illnesses include rapid ascent, exertion, prior history, age under 50, and underlying lung/heart conditions. (3) Treatment depends on the illness but may include descent, oxygen, medications like dexamethasone or nifedipine, and hyperbaric bags that simulate lower altitudes.