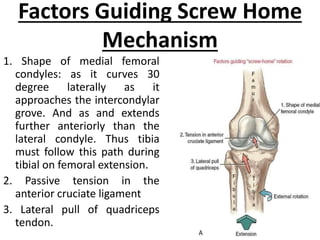
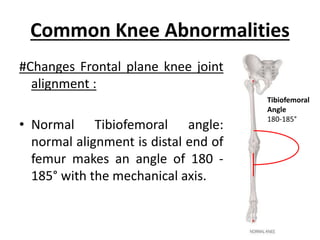
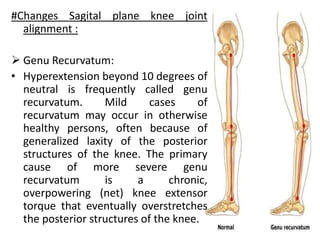
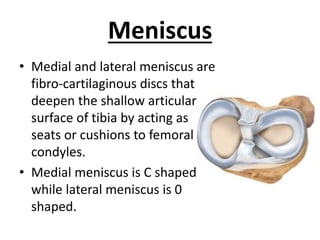
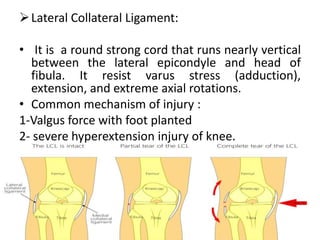
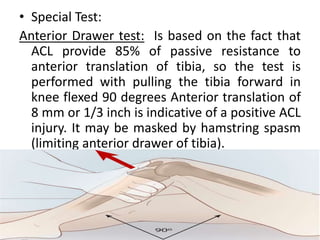
The document outlines the pathomechanics of the knee joint, detailing its anatomical structure, various mechanisms like the screw home mechanism, and the unlocking mechanism. It also discusses common knee abnormalities such as genu valgum and genu varum, as well as injuries to the meniscus and ligaments, including the anterior and posterior cruciate ligaments. Additionally, it covers patellofemoral disorders and their implications on knee function and rehabilitation considerations.