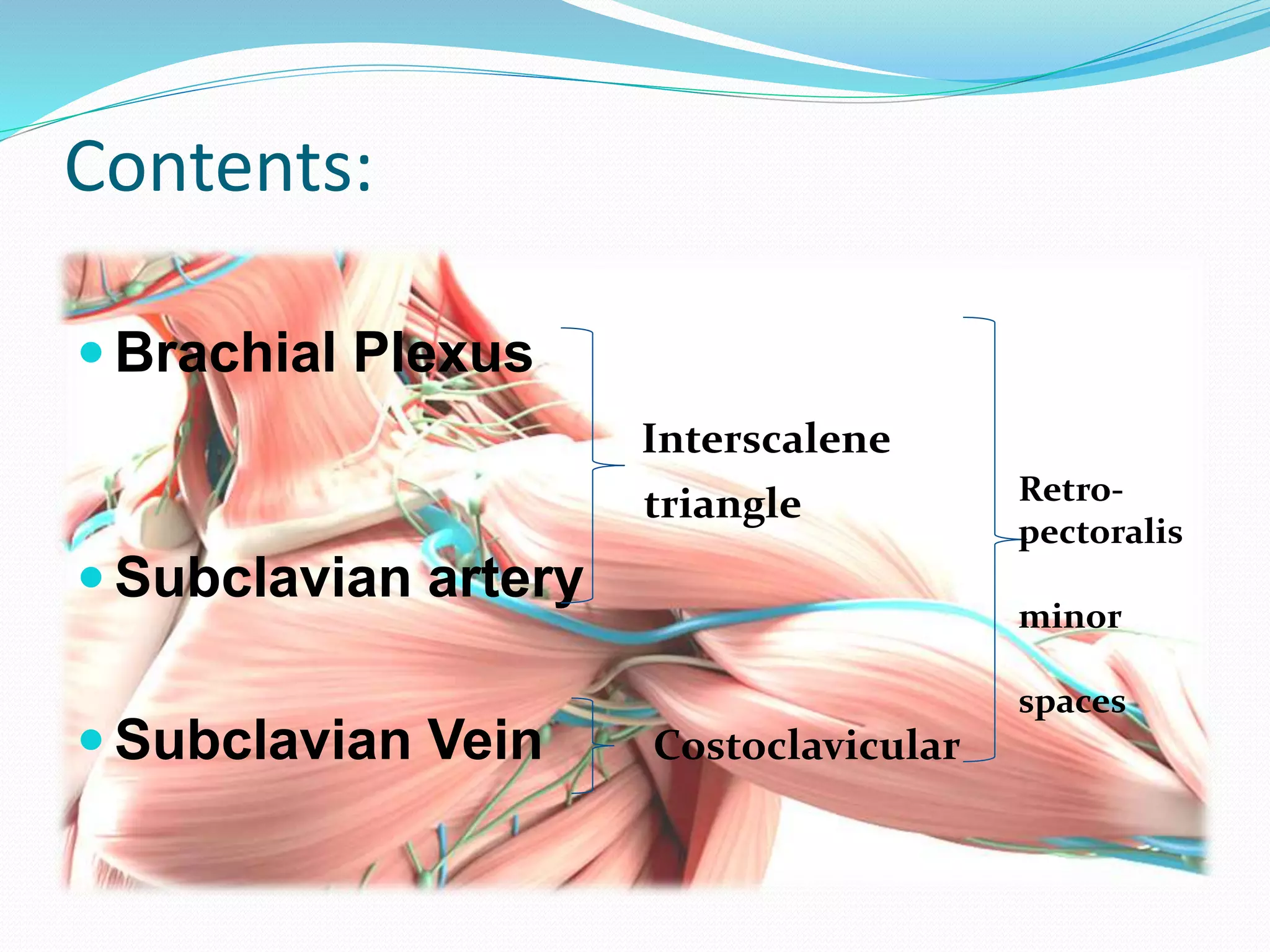
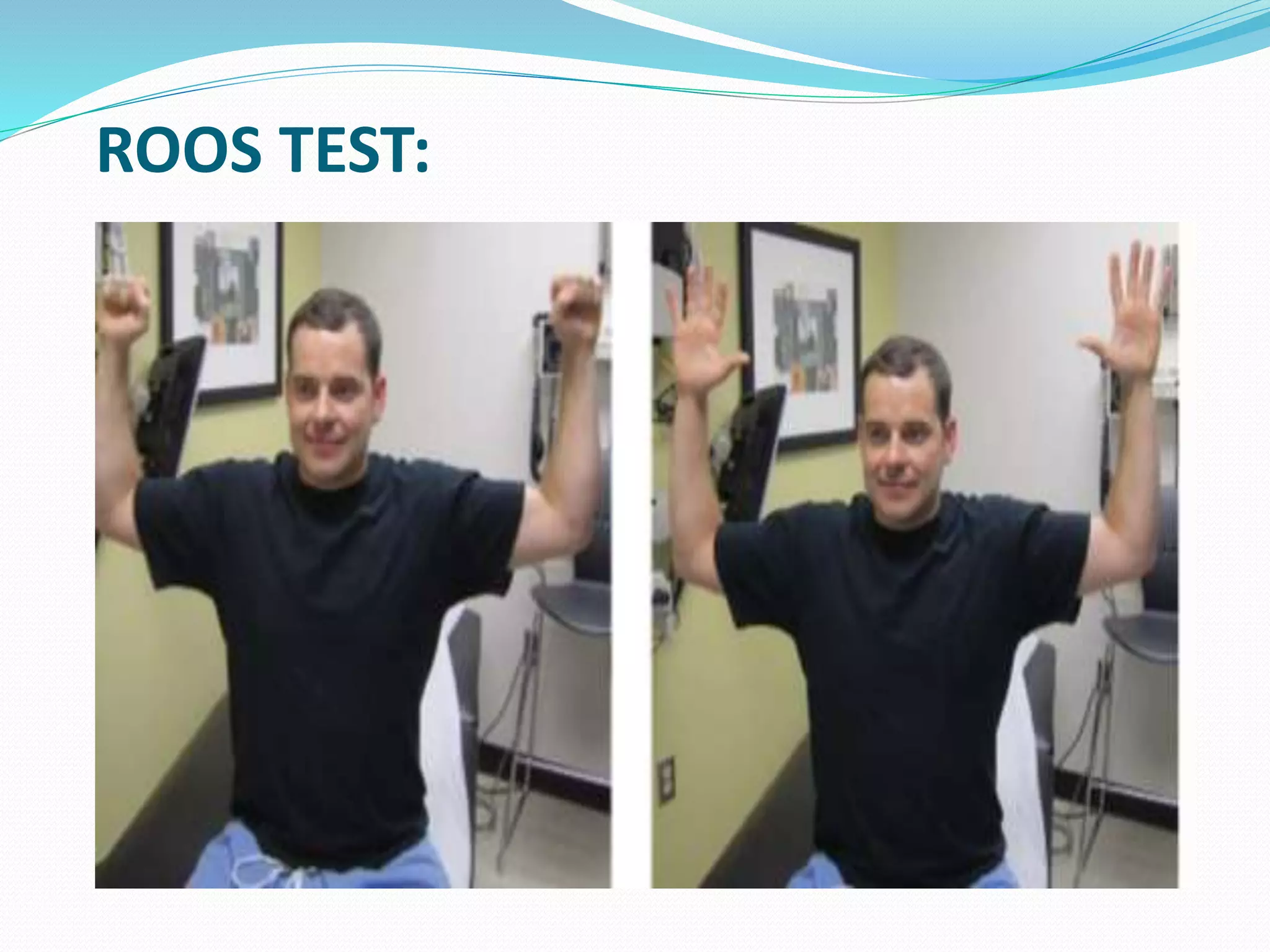
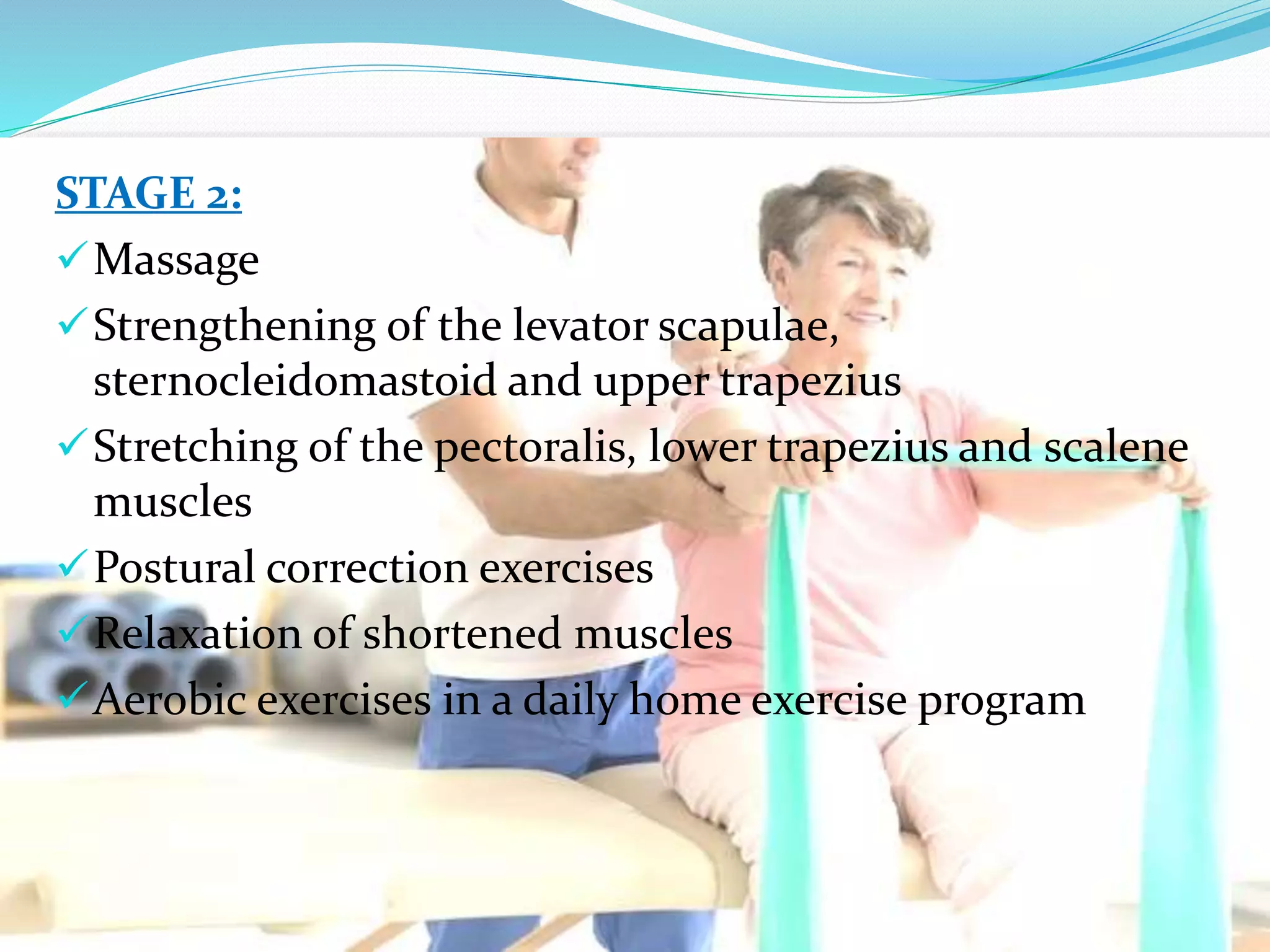
This document presents information on thoracic outlet syndrome (TOS). It begins with definitions and descriptions of the thoracic outlet anatomy. It then discusses the contents and structures that pass through the thoracic outlet including the brachial plexus, subclavian artery, and subclavian vein. Etiology and classifications of TOS are outlined. The document provides details on physical exams used to diagnose TOS and differential diagnoses. Conservative management including exercises and manual therapy techniques are explained. Two research articles on manual therapy and scalene injections/stretching for TOS are summarized. Reference sources are listed at the end.