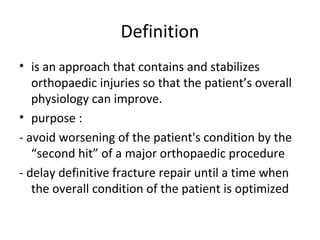
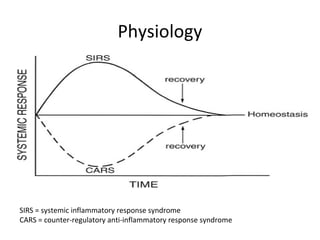
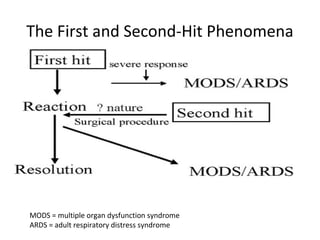
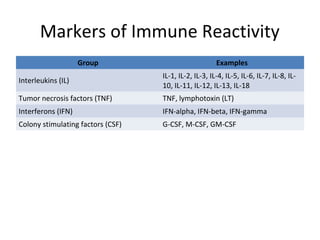
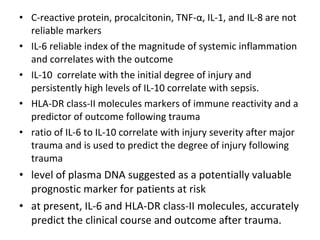
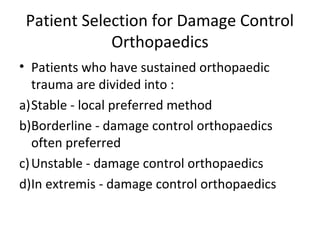
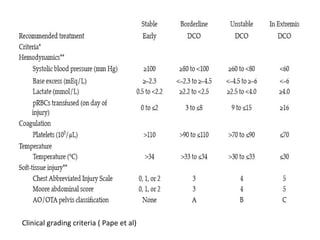
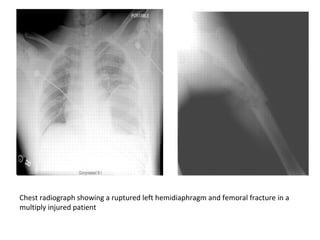
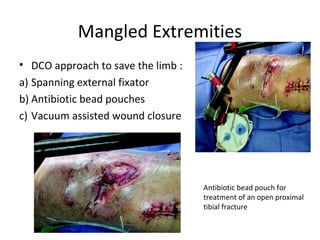
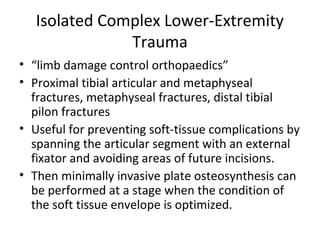
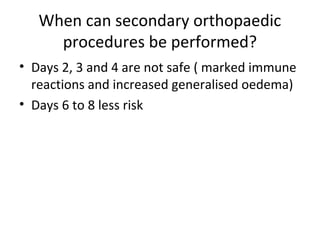
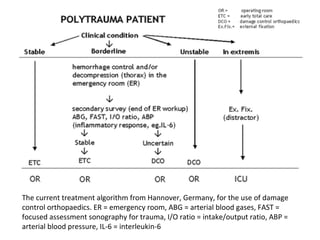
Damage control orthopaedics is an approach that temporarily stabilizes orthopaedic injuries to avoid worsening a patient's condition through definitive surgery. It aims to delay repair until the patient's physiology improves. Key indications include unstable pelvic fractures, femoral fractures in patients with chest injuries, and mangled or isolated lower extremity trauma. Temporary external fixation is often used followed by staged definitive surgery once the patient stabilizes in 2-8 days. Monitoring inflammatory markers like IL-6 helps determine when secondary procedures can be safely performed.