The document provides guidelines for assessing and managing patients with polytrauma from the pre-hospital phase through discharge, including conducting a primary and secondary survey to identify and treat life-threatening injuries, determining appropriate patient transfer based on injury severity, and providing continued monitoring and care through definitive treatment and recovery. Key aspects of the primary survey are evaluating the airway, breathing, circulation, disability, and exposure to address issues like tension pneumothorax, head injuries, hemorrhage, and potential for organ dysfunction.

![Definition
• The term ‘polytrauma’ was first used by Tscherne et al., in 1966 for
patients that demonstrated a combination of at least 2 ‘severe injuries
of the head, chest or abdomen’, or ‘one of them in association with an
extremity injury’.
• Trentz in 1999 defined Polytrauma is a syndrome of multiple injuries
exceeding a defined severity (Injury Severity Score [ISS] >17) with
sequential systemic reactions that can lead to dysfunction or failure of
remote organs and vital systems, which have not themselves been
directly injured.
• Oestern, Hans-Jörg; Trentz, Otmar; Uranues, Selman (2014). General Trauma Care and Related Aspects || Polytrauma: Pathophysiology, Priorities, and
Management. , 10.1007/978-3-540-88124-7(Chapter 5), 69–76. doi:10.1007/978-3-540-88124-7_5](https://image.slidesharecdn.com/polytrauma-assessmentandmanagementtilldischarge-230330044446-83a0b94a/75/Polytrauma-Assessment-and-management-till-discharge-pptx-3-2048.jpg)


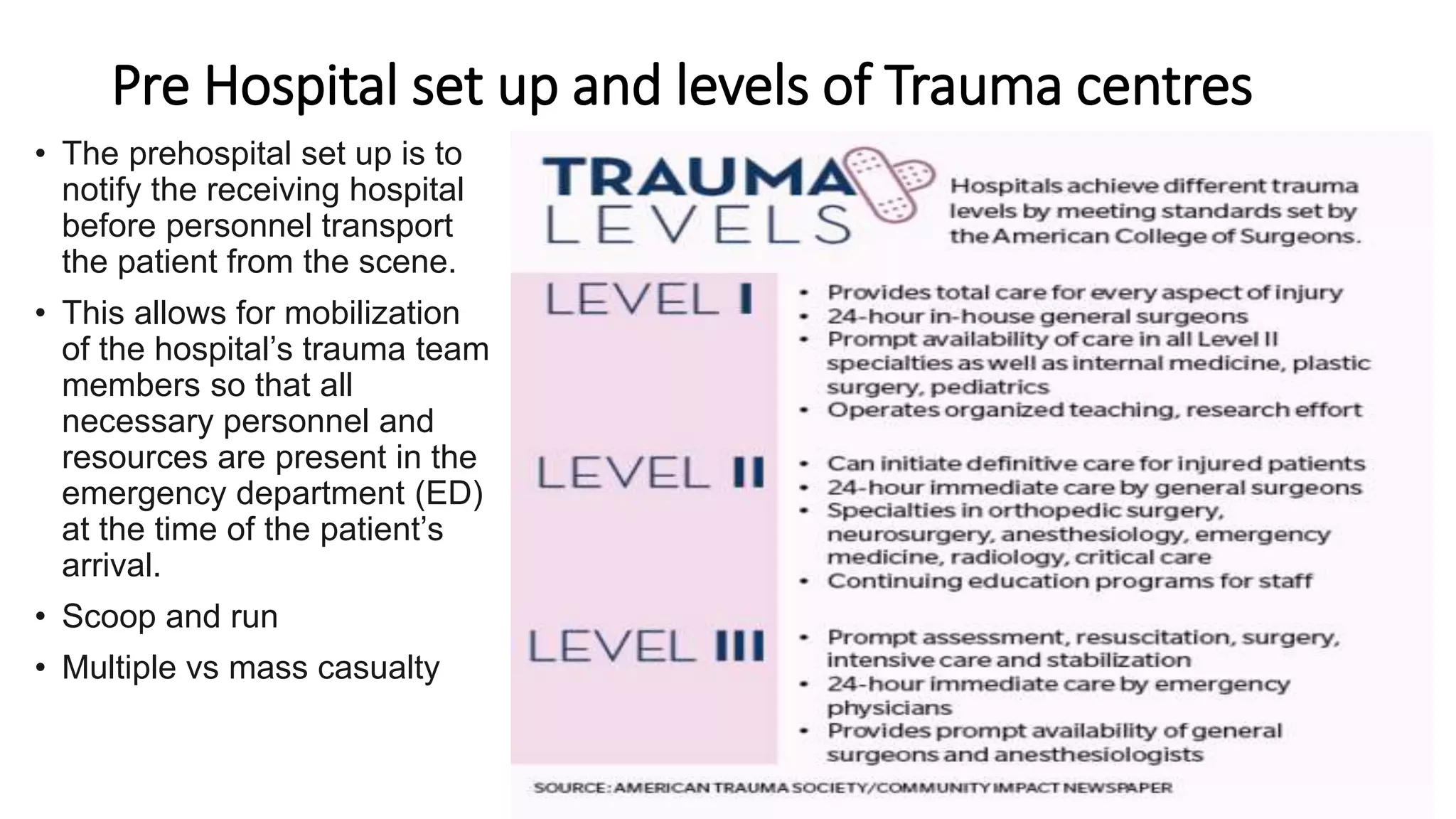






![Canadian C-spine rule
To be more selective in use of radiography in alert and stable
trauma patients.
Design: Prospective cohort study conducted from October 1996 to April
1999, sample of 8924 adults (mean age, 37 years) with blunt trauma to the
head/neck, stable vital signs, and a GCS of 15.
151 patients had (1.7%) had C-spine injury.
The resultant model and final Canadian C-Spine Rule comprises 3 main
questions:
(1) is there any high-risk factor present that mandates radiography
(2) is there any low-risk factor present that allows safe assessment of range
of motion
(3) is the patient able to actively rotate neck 45 degrees to the left and
right?
By cross-validation, this rule had 100% sensitivity (95% confidence interval
[CI], 98%-100%) and 42.5% specificity (95% CI, 40%-44%) for identifying
151 clinically important C-spine injuries. The potential radiography ordering
rate would be 58.2%.
The Canadian C-Spine rule of radiography in alert and stable trauma patients. JAMA
2001;286:1841–1848.](https://image.slidesharecdn.com/polytrauma-assessmentandmanagementtilldischarge-230330044446-83a0b94a/75/Polytrauma-Assessment-and-management-till-discharge-pptx-14-2048.jpg)