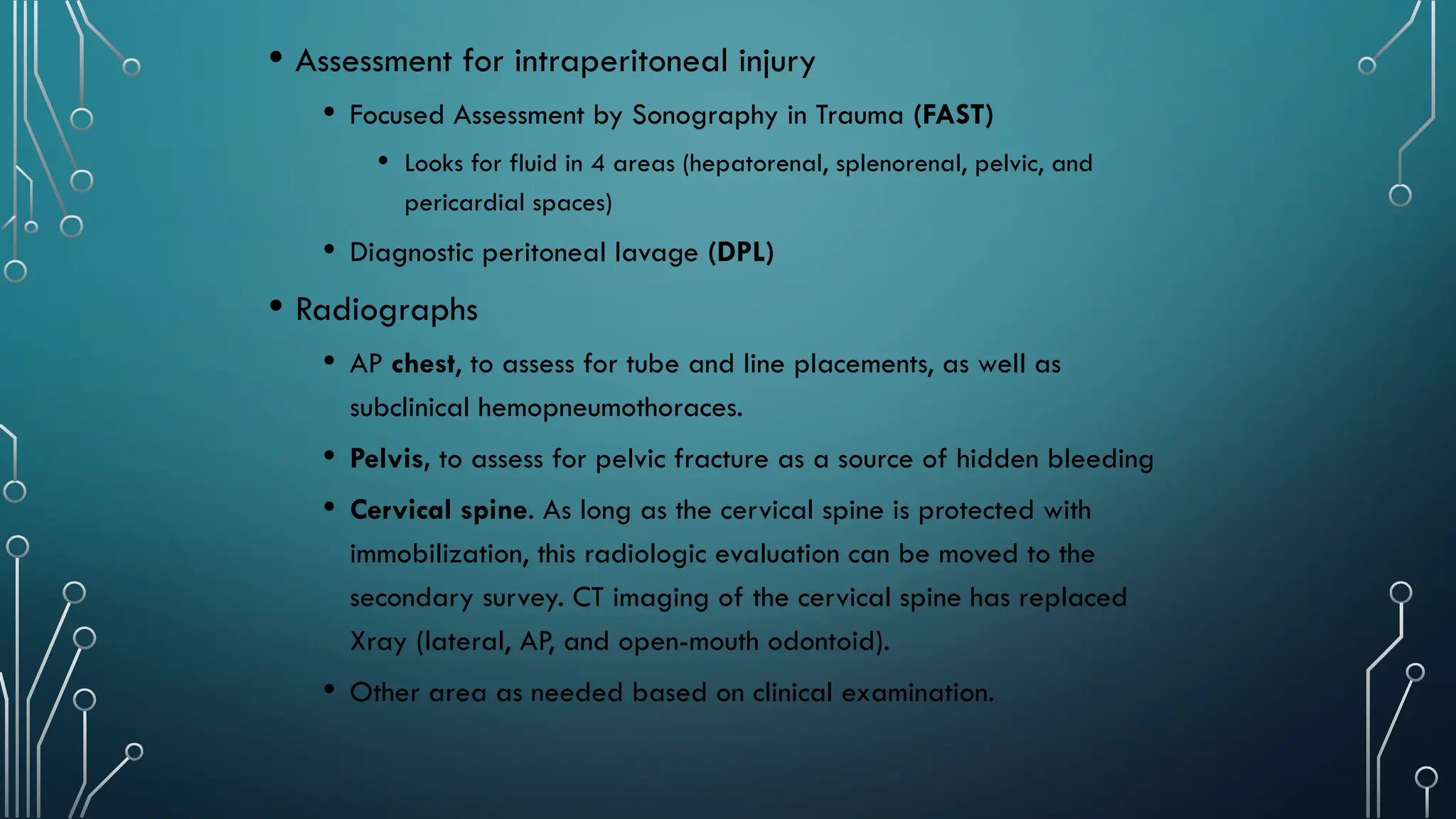
The document details a case presentation of a 20-year-old mill worker, Amir Waseem, who suffered severe back pain due to a fall. A comprehensive primary and secondary trauma assessment was conducted, revealing no life-threatening conditions, but signs of spine tenderness and bruising, leading to conservative management with IV fluids and pain medication. It also outlines the principles and steps of Advanced Trauma Life Support (ATLS), emphasizing the importance of immediate assessment and intervention in trauma cases.