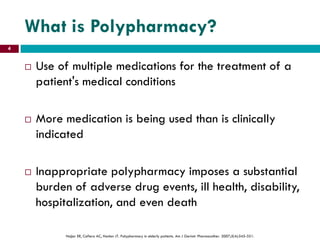
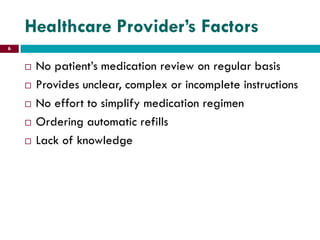
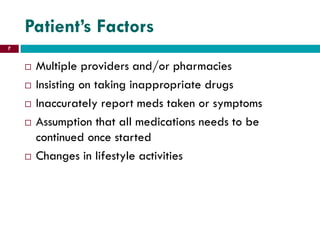
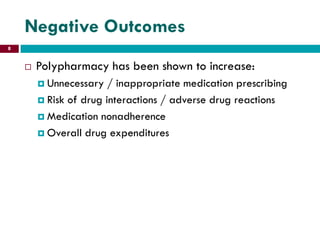
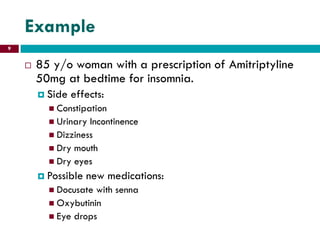
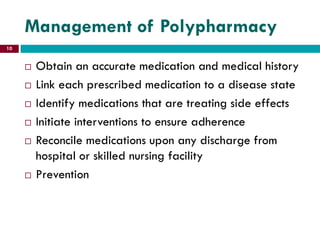
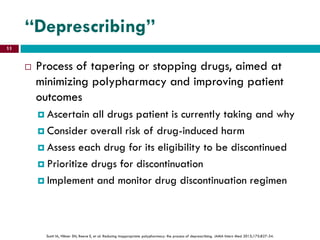
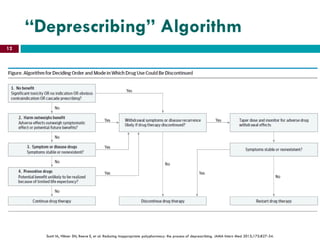
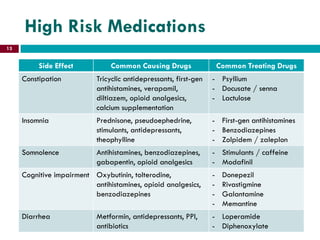
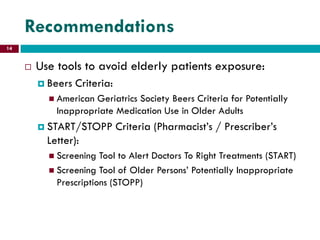
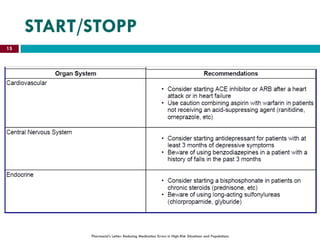
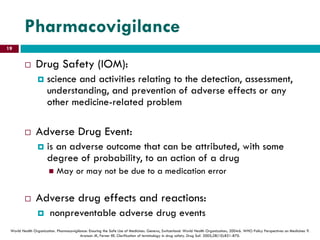
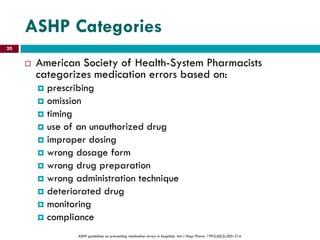
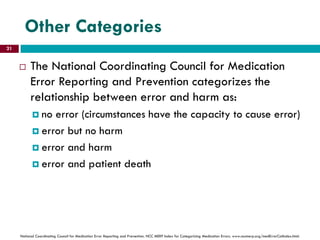
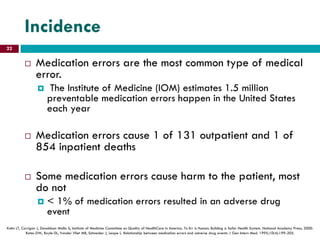
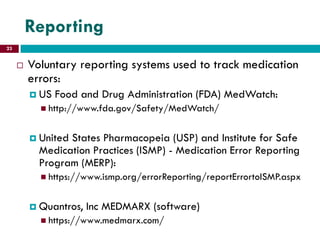
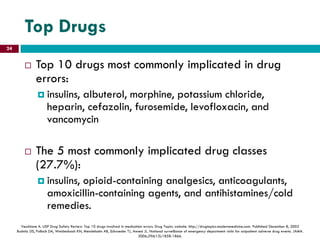
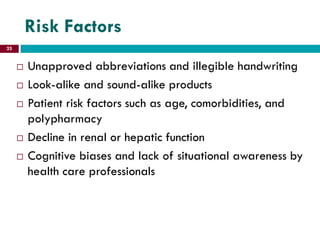
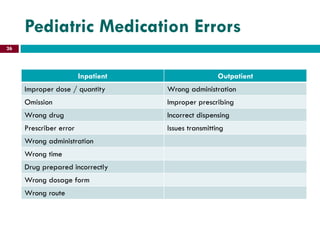
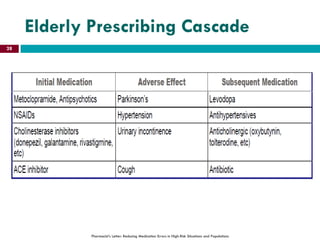
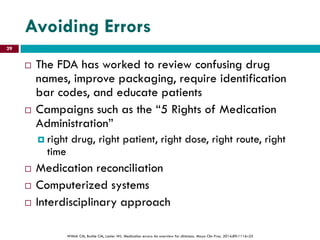
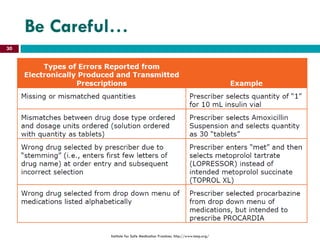
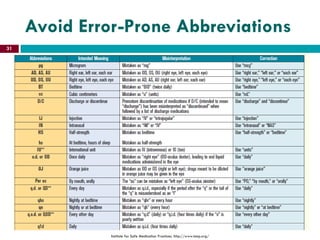
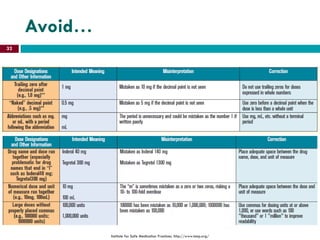
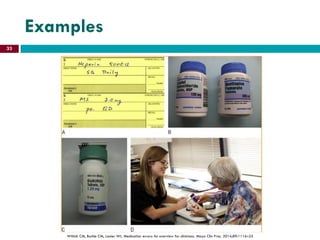
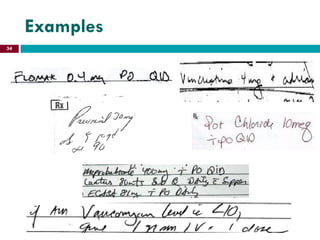
This document discusses polypharmacy and medication errors. It begins by defining polypharmacy as the use of multiple medications where more are being used than clinically indicated. Polypharmacy can increase the risk of drug interactions and adverse events. Common risk factors for polypharmacy include the elderly, multiple comorbidities, recent hospitalization, and multiple physicians or pharmacies. Medication errors are also defined as any error in the medication use process and examples are provided. Reporting systems for medication errors and the most commonly implicated drug classes and individual drugs are outlined. Risk factors for errors and recommendations to reduce polypharmacy and errors are presented.