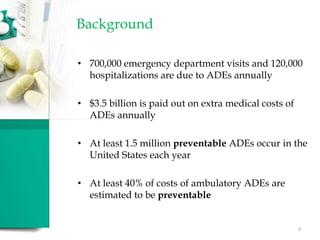
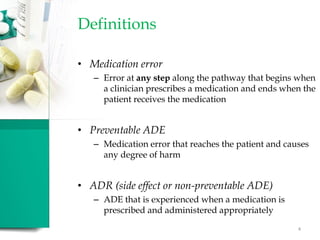
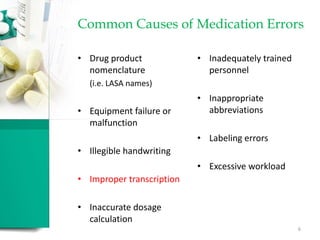
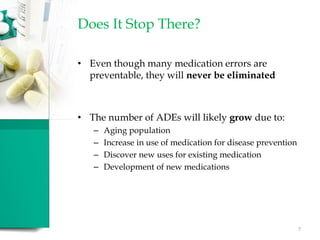
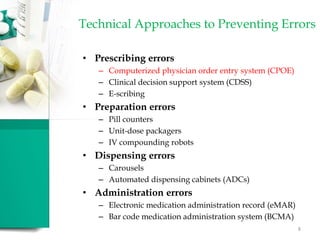
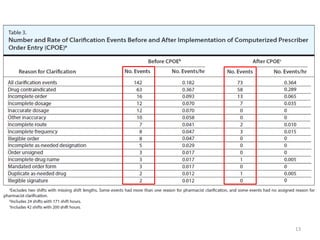
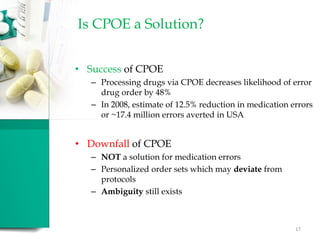
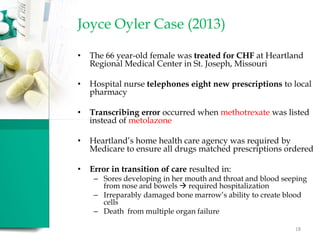
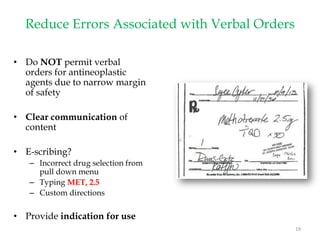
The document discusses the significant issue of medication errors, emphasizing their causes, impacts, and prevention strategies, including the implementation of computerized physician order entry systems (CPOE) combined with clinical decision support systems (CDSS). It highlights that while medication errors are common and costly, the integration of technology can reduce these errors; however, challenges such as order ambiguity and the need for ongoing system optimization persist. The proposed addition of a 'sixth right' to medication ordering—right indication—aims to further enhance patient safety, though it brings potential complexities in implementation.