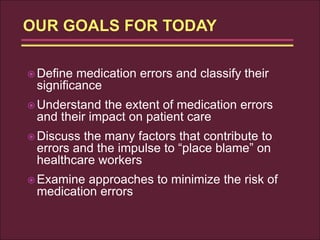
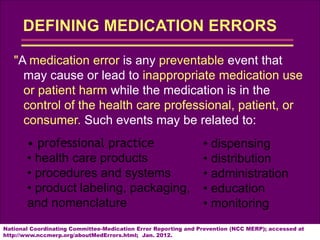
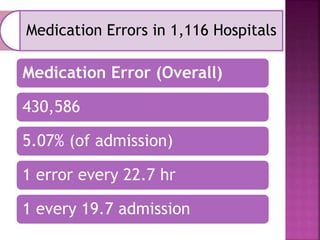
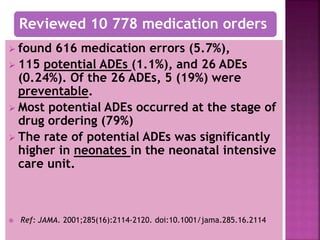
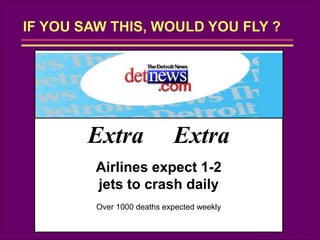
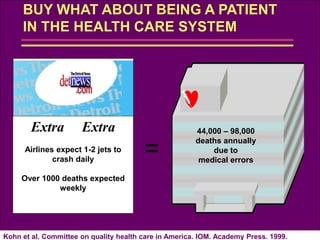
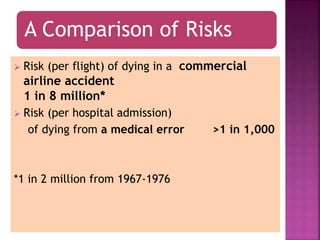
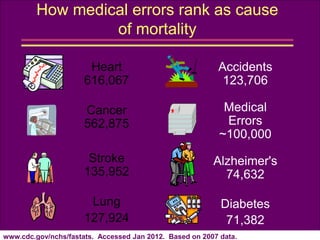
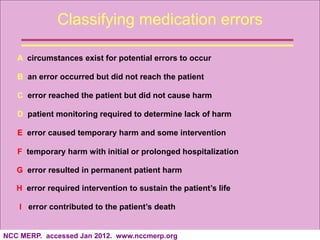
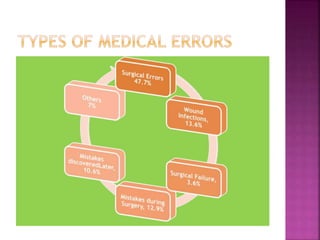
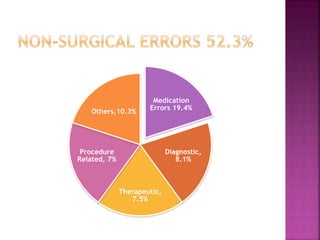
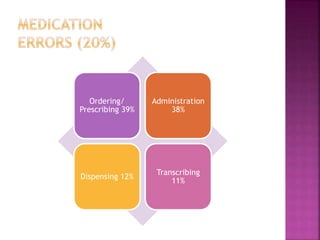
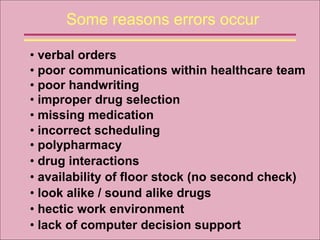
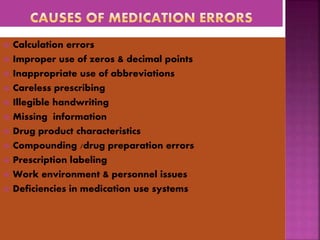
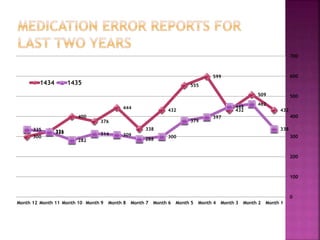
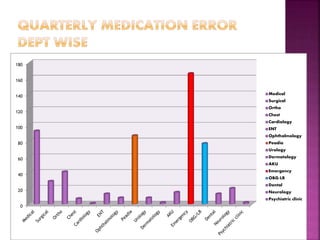
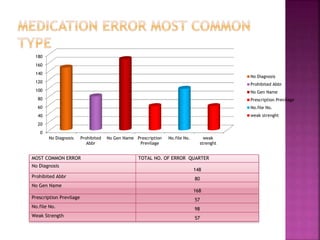
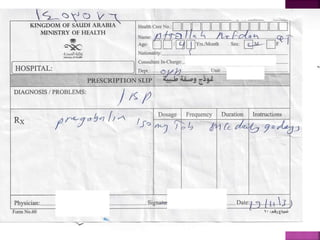
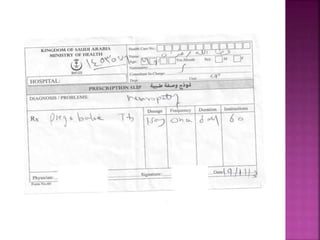
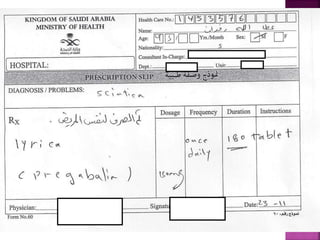
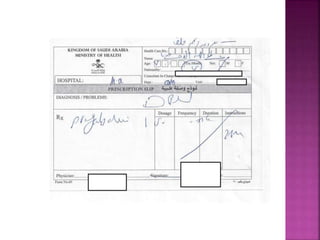
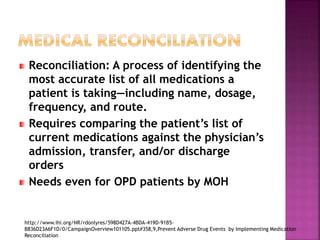
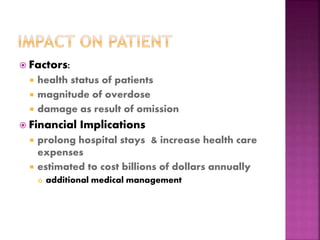
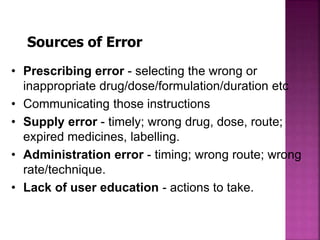
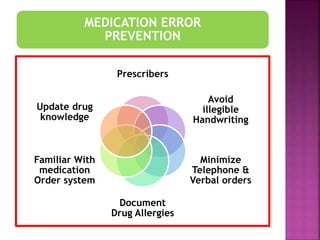
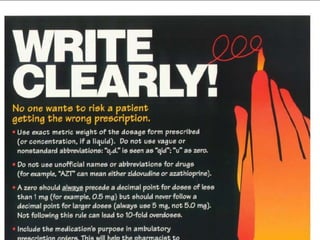
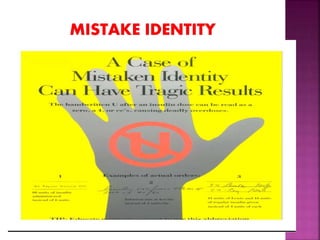
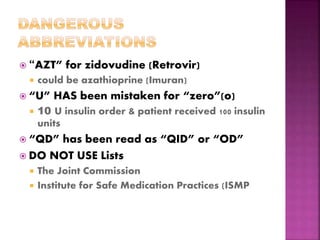
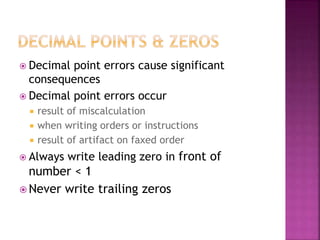
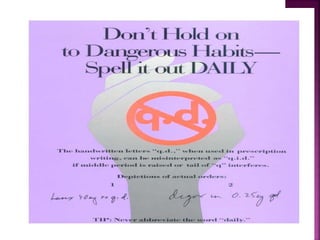
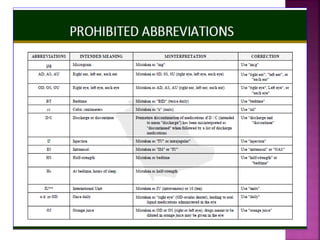
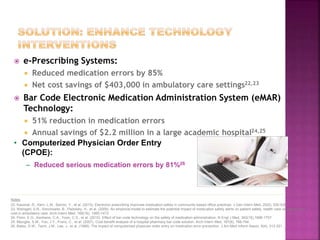
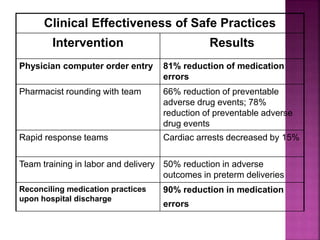
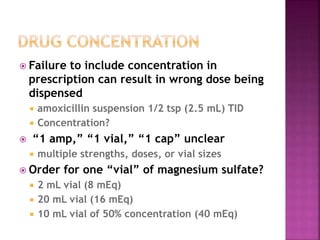
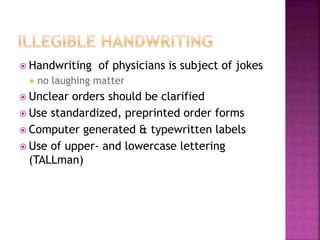
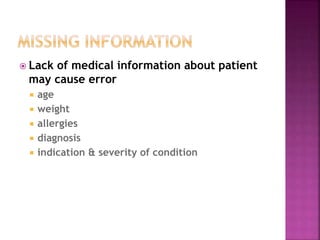
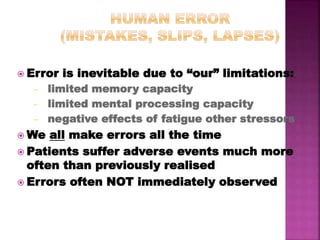
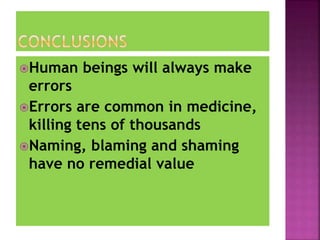
This document outlines a strategic plan to minimize medication errors in healthcare. It begins by defining medication errors and classifying their significance. It then discusses the extent of medication errors, finding they occur in 1 in every 19 hospital admissions. The document examines the many factors that contribute to errors, including poor communication, look-alike drug names, and busy work environments. It also presents approaches to reduce errors such as electronic medical records, barcoding medications, and computerized physician order entry, which can reduce serious medication errors by up to 81%. The goal of the plan is to understand, prevent, and minimize medication errors to improve patient safety.