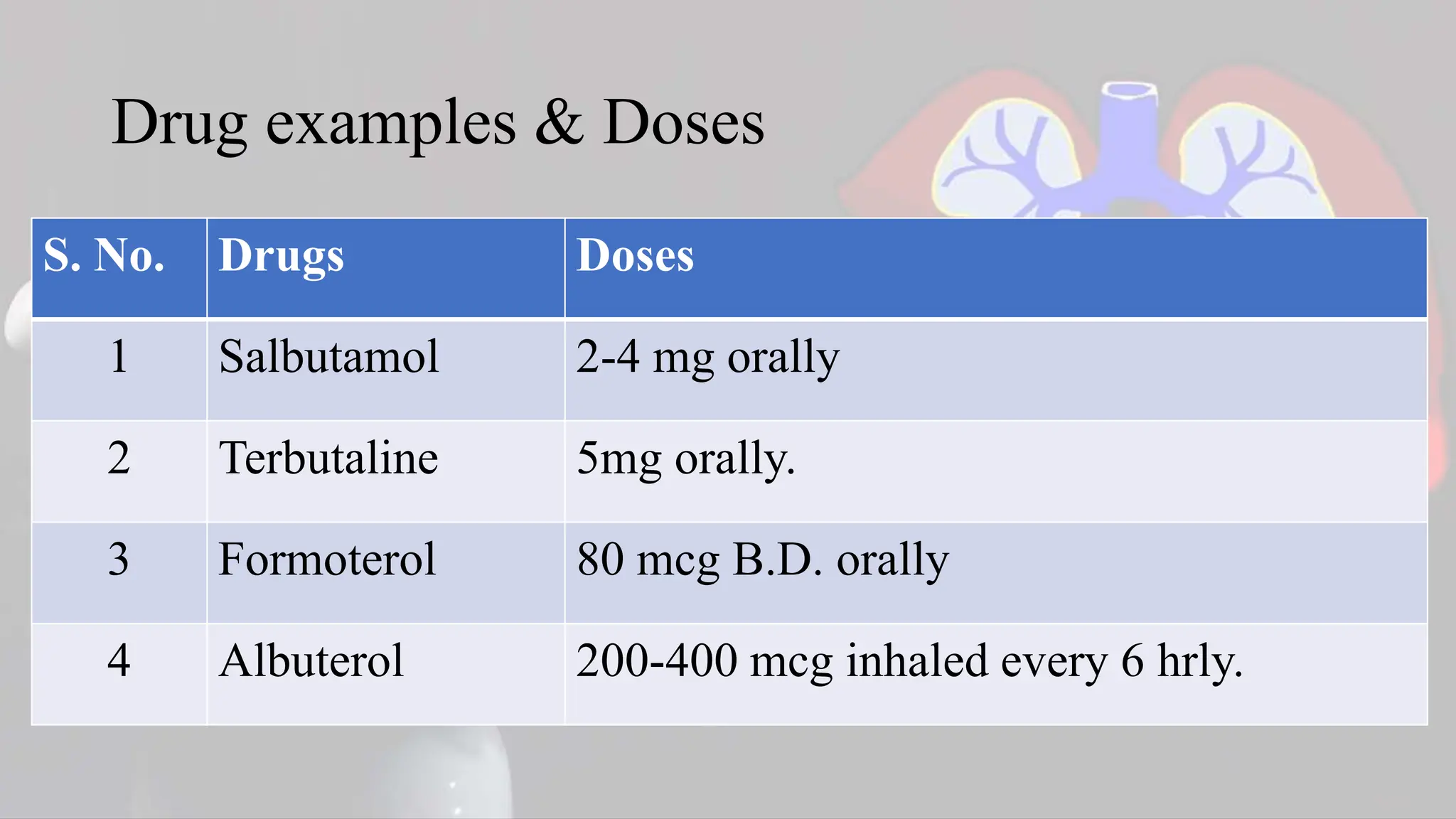
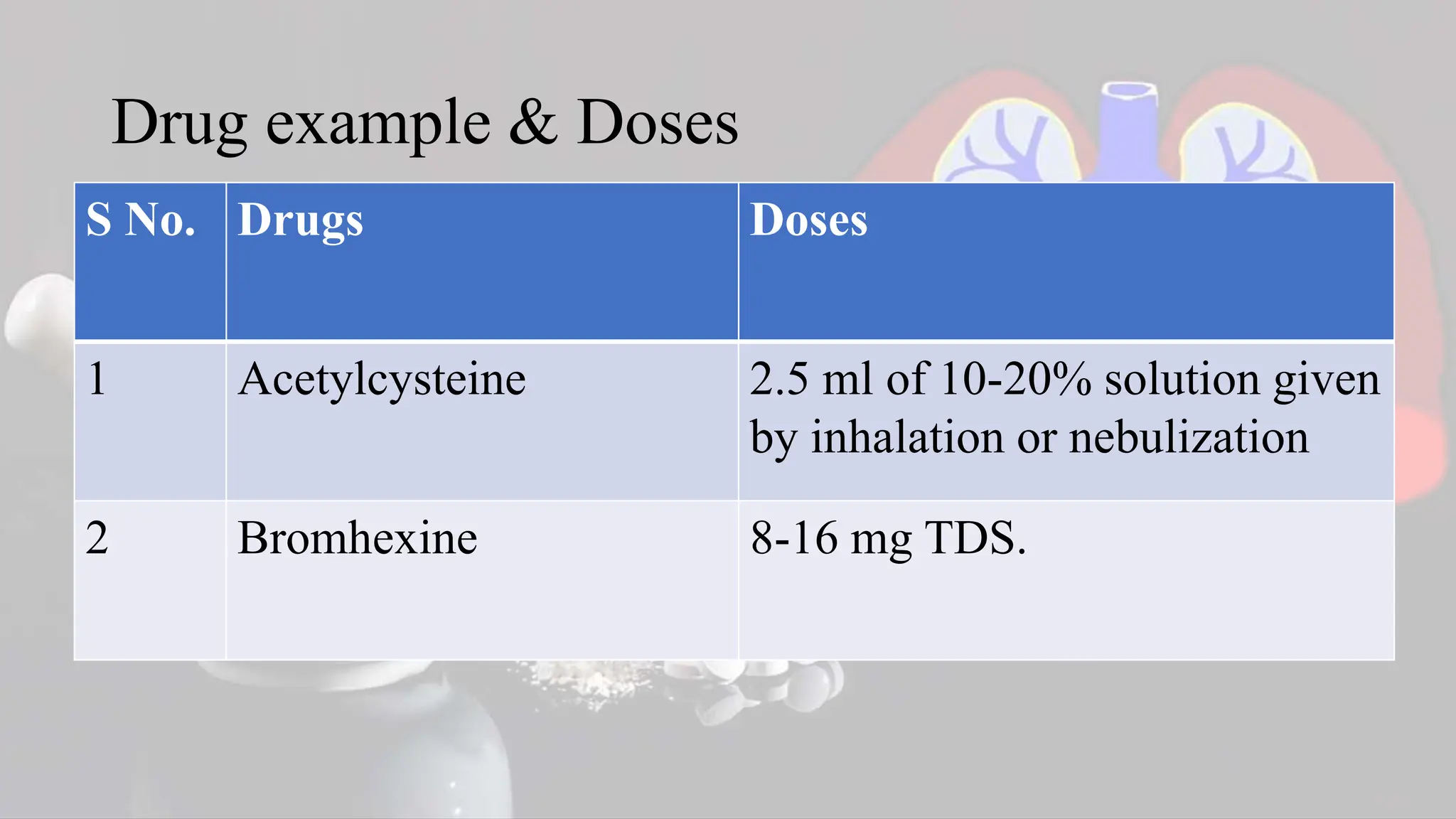
The document provides a comprehensive overview of drugs used for the respiratory system, including categories like bronchodilators, anticholinergics, mast cell stabilizers, corticosteroids, antihistamines, mucolytics, decongestants, and cough medications, along with their mechanisms of action, uses, contraindications, adverse effects, drug interactions, and nursing responsibilities. Specific drugs and dosages are listed for each category, highlighting key considerations for their use in treating respiratory conditions such as asthma, bronchitis, and allergic reactions. It emphasizes the importance of nursing responsibilities in monitoring patients and educating them on proper medication use.