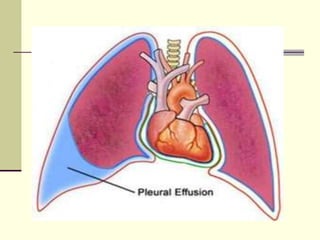
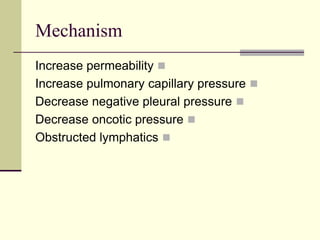
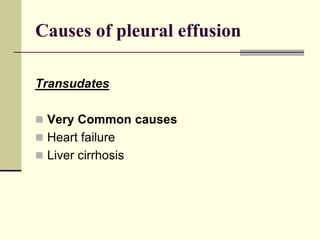
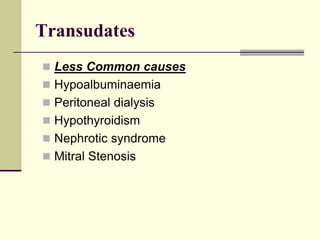
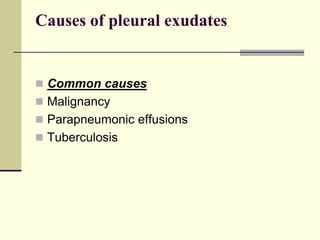
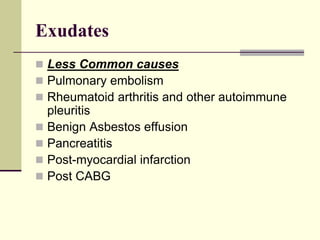
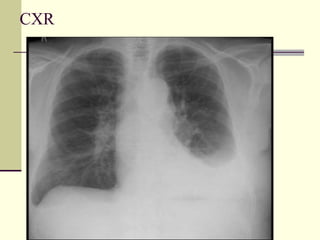
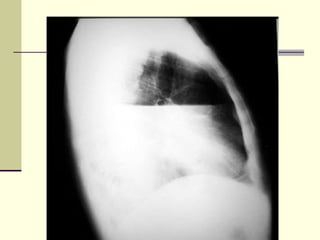
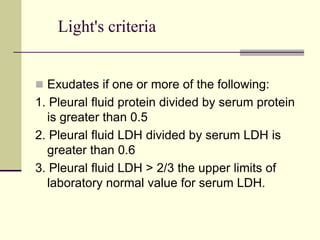
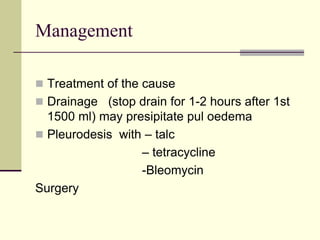
The document outlines the mechanisms and types of pleural effusions, distinguishing between transudates and exudates and their common causes such as heart failure and malignancy. It emphasizes clinical assessment through history, physical examination, and diagnostic methods such as CXR and pleural aspiration using Light's criteria for classification. Management focuses on treating the underlying cause, drainage of effusion, and potential surgical interventions.