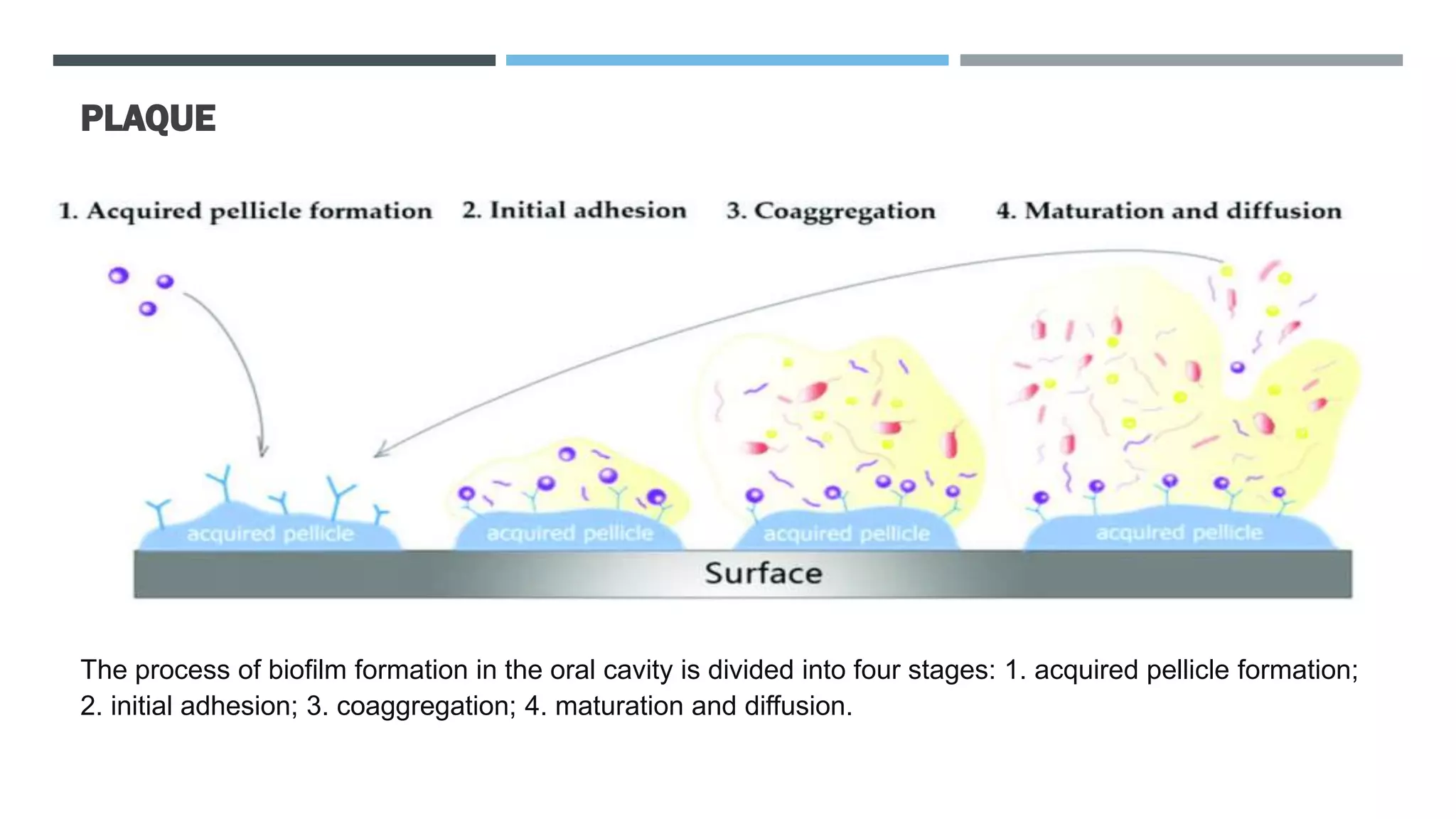
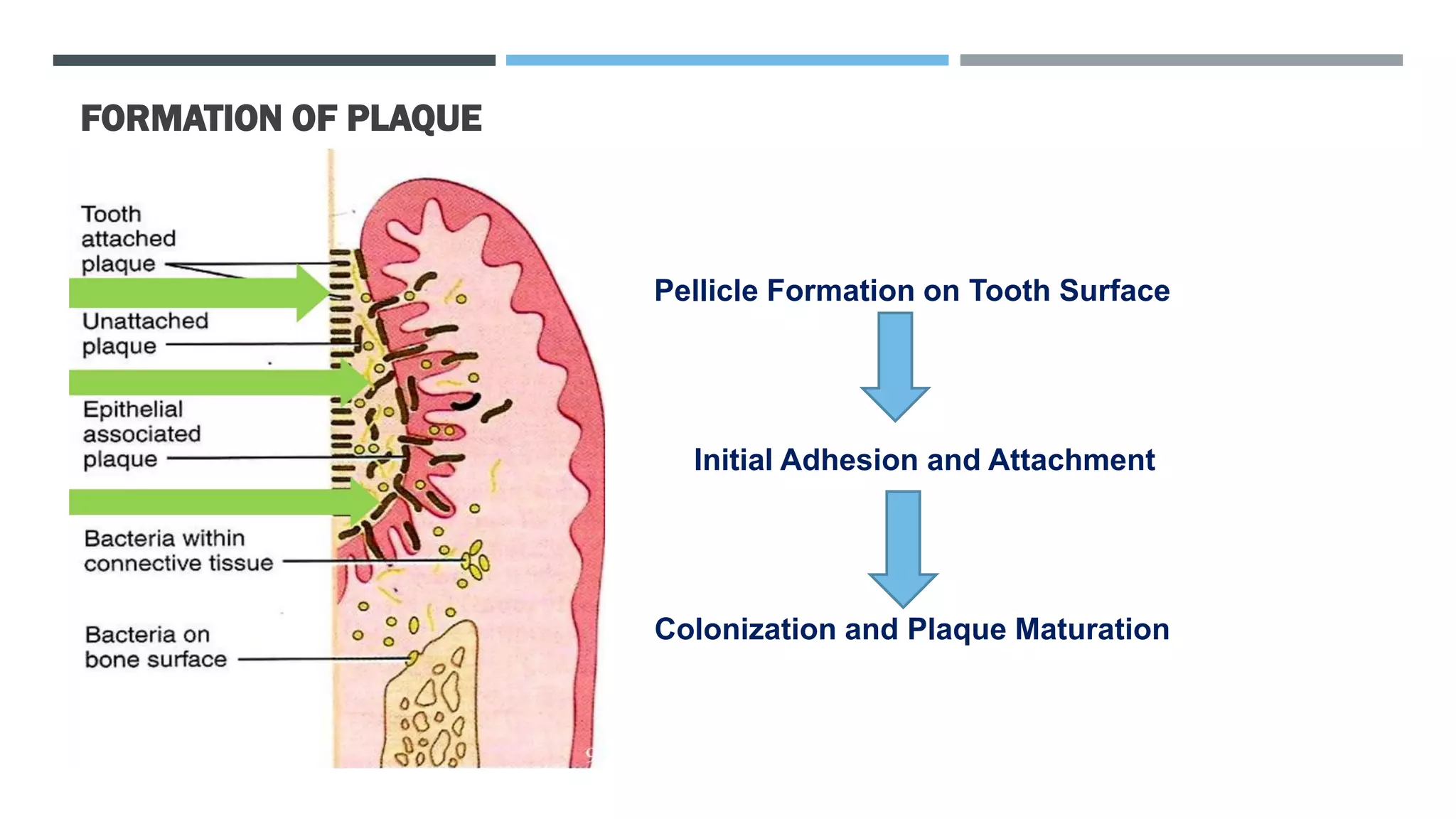
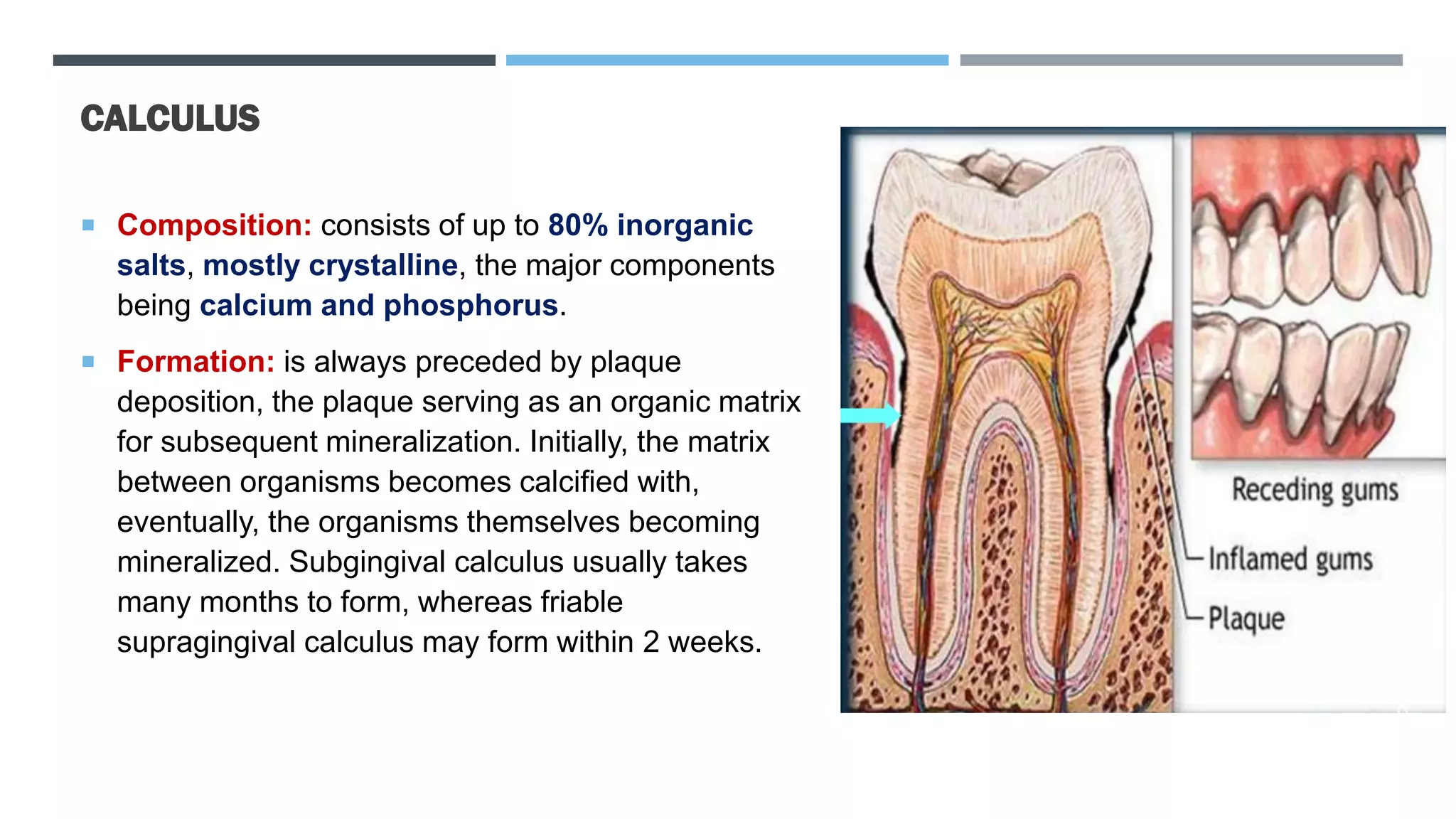
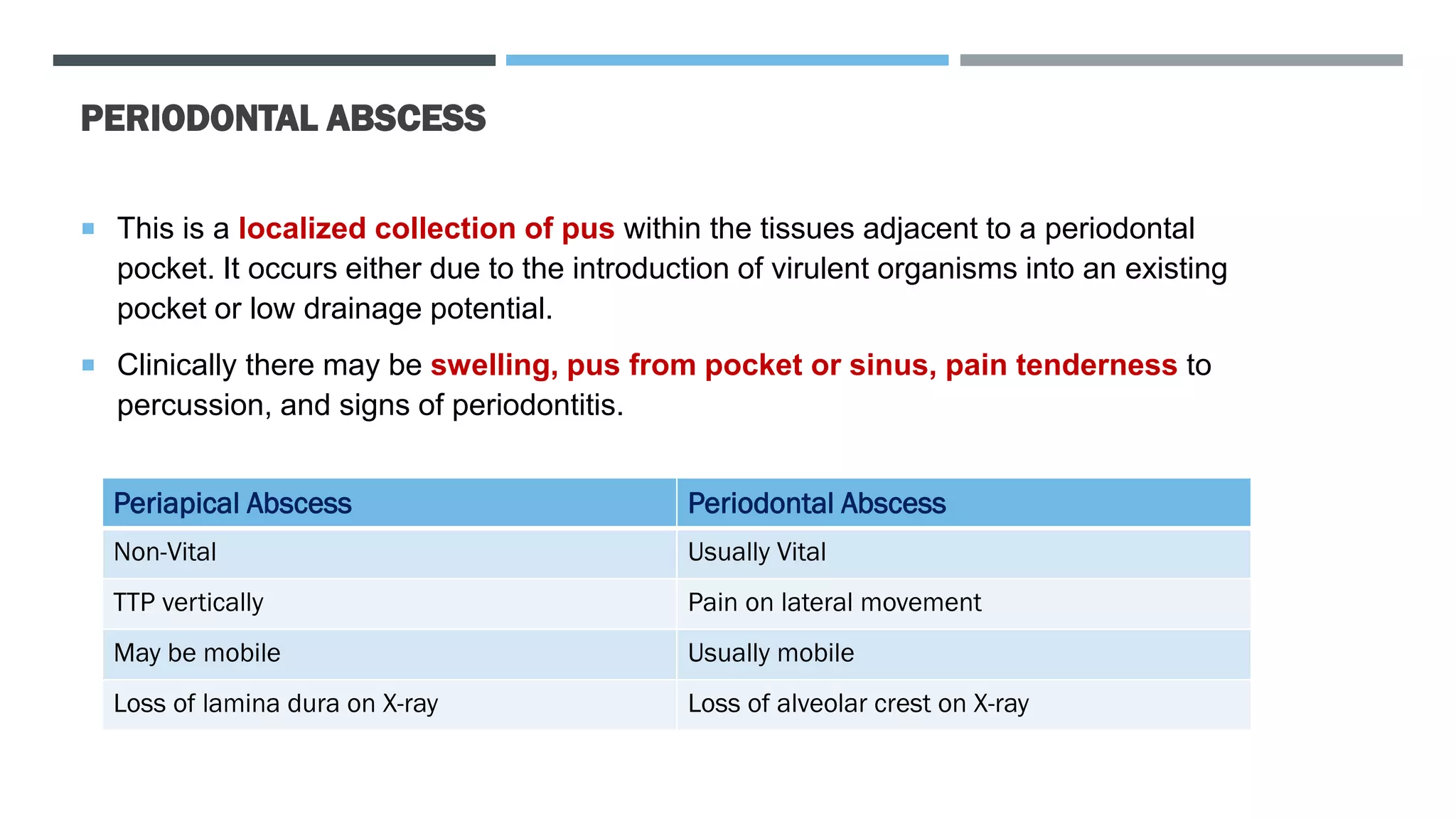
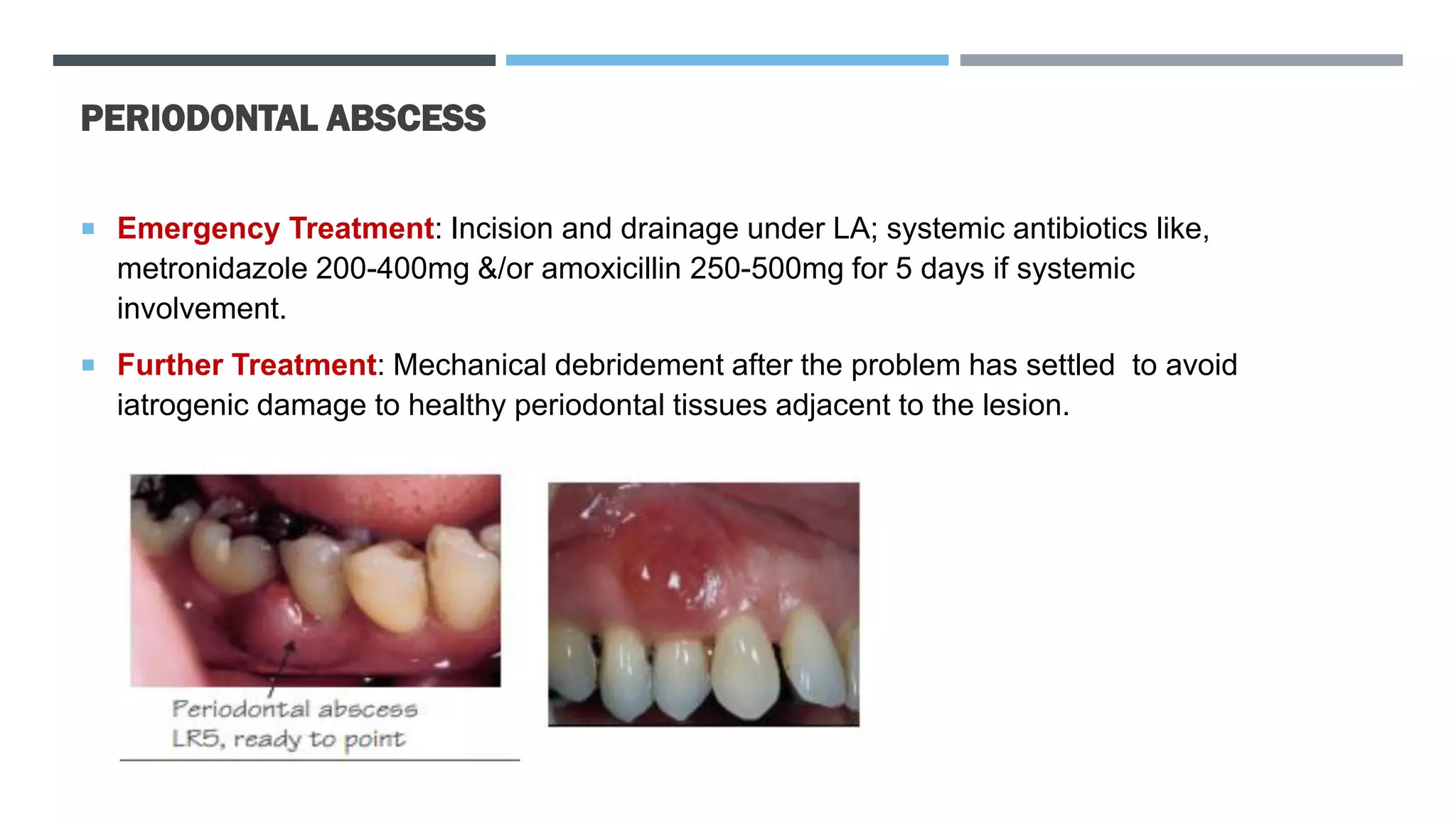
This document provides information on periodontal diseases including their etiology, plaque, calculus, and periodontal abscesses. It discusses how plaque biofilm builds up in 4 stages and leads to gingivitis. It then explains how the inflammatory response creates an environment for more bacteria to colonize and cause periodontitis. It details the formation of supragingival and subgingival calculus from mineralization of plaque. Finally, it provides information on diagnosing and treating periodontal abscesses.