This document provides an overview of suppositories including:
- Definition: Suppositories are solid or semi-solid dosage forms meant to melt or dissolve in body cavities to deliver medication locally or systemically.
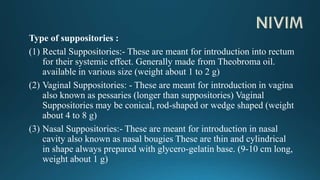
- Types include rectal, vaginal, nasal, urethral, and ear suppositories.
- Advantages include ease of administration to certain patients and targeted delivery to specific body cavities. Disadvantages include potential embarrassment and need for special storage conditions.
- Common bases include fatty bases like cocoa butter and hydrophilic bases like gelatin that melt at body temperature to release the drug.