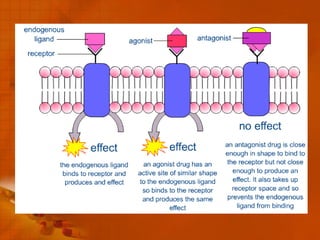
Drugs and the Body discusses the pharmacokinetics and pharmacodynamics of how drugs act on the body. Pharmacokinetics describes the absorption, distribution, metabolism and excretion of drugs in the body. Pharmacodynamics examines how drugs produce their effects by interacting with receptor sites or replacing missing chemicals. Nursing management of drug administration involves ensuring the "rights" of giving the right drug to the right patient via the right route and dose. The nursing process - which includes assessment, nursing diagnosis, planning, interventions and evaluation - is used to properly manage a patient's drug therapy.