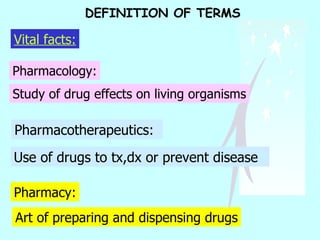
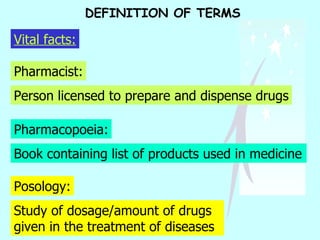
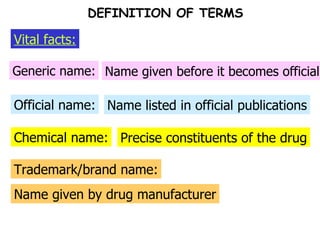
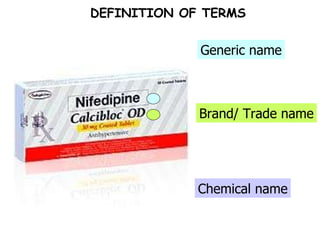
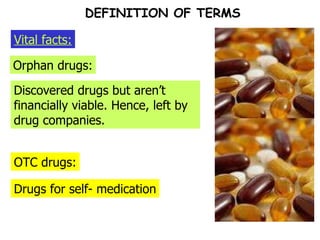
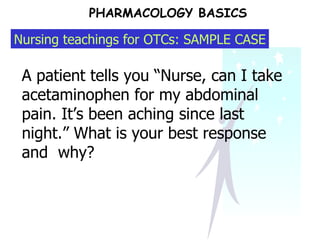
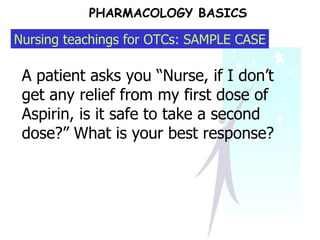
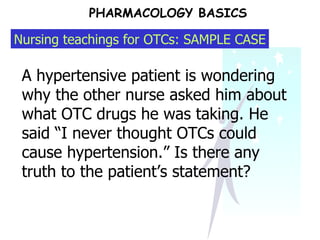
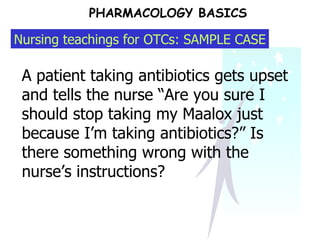
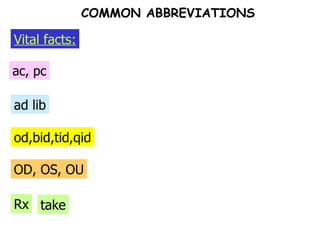
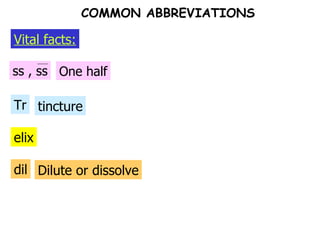
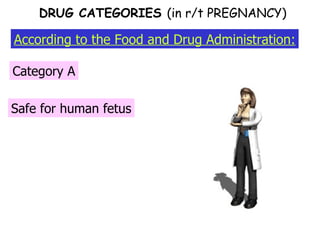
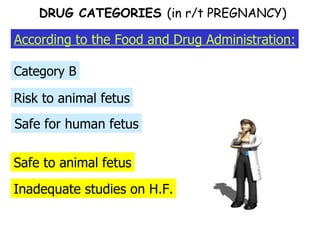
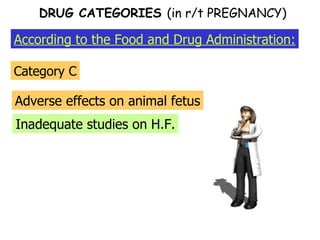
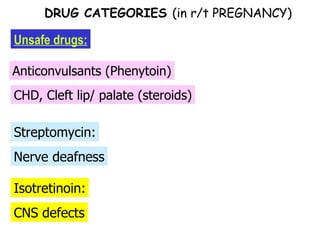
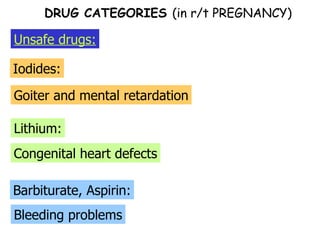
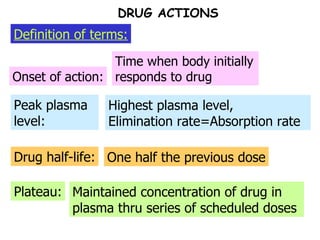
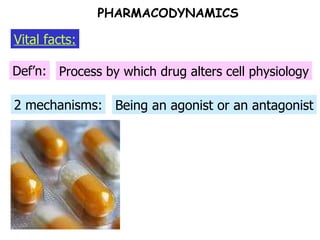
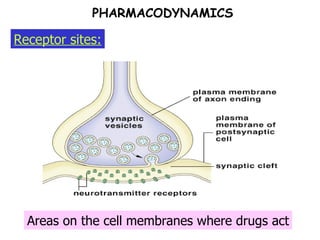
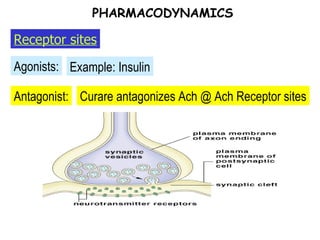
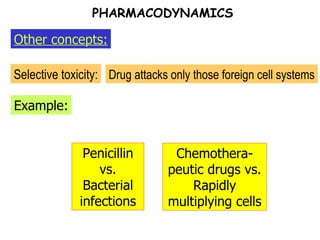
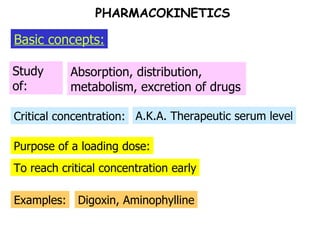
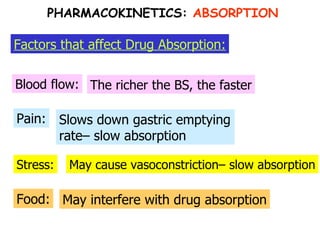
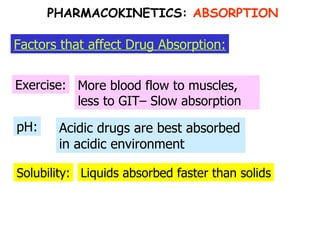
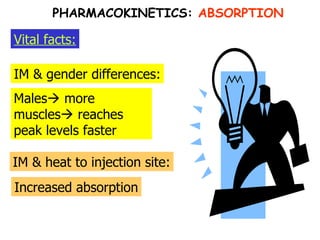
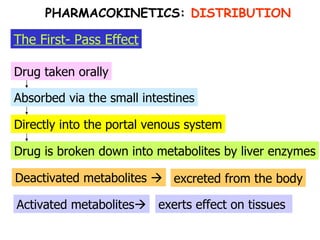
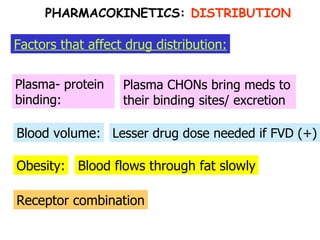
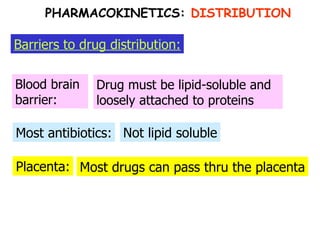
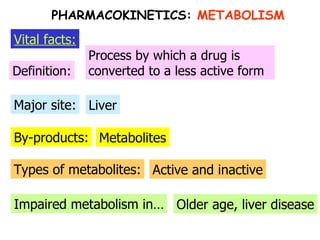
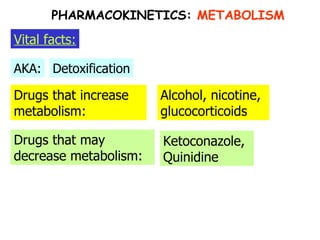
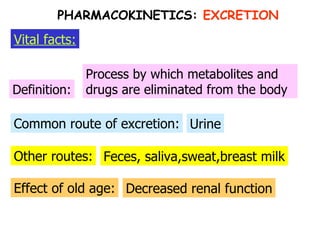
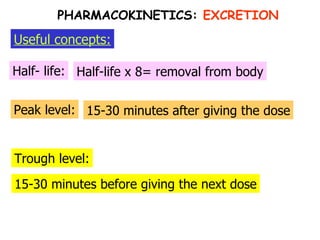
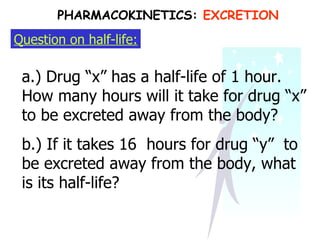
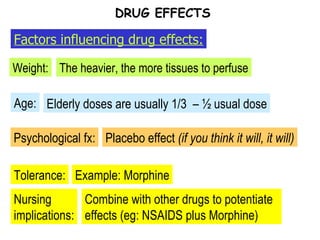
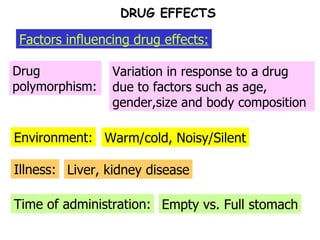
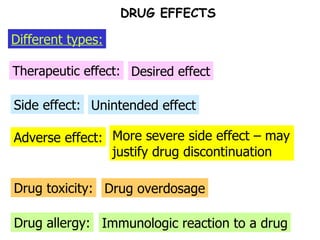
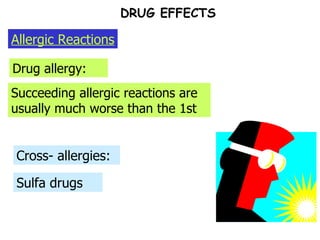
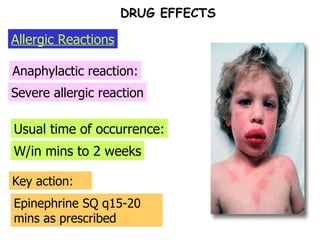
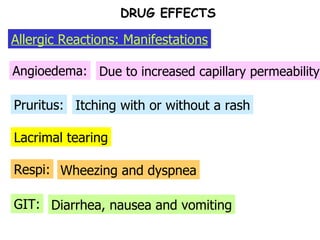
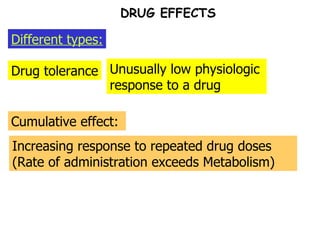
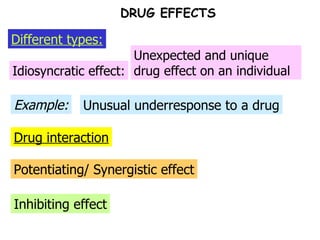
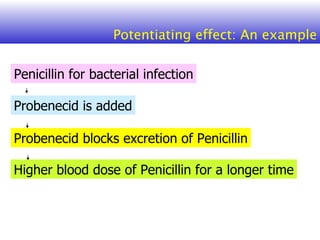
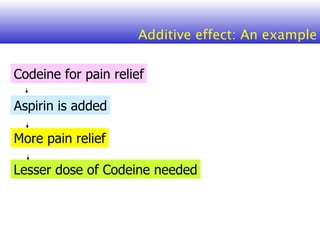
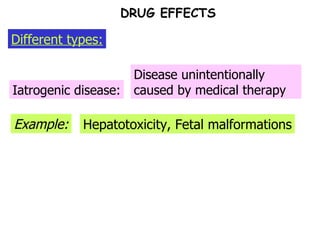
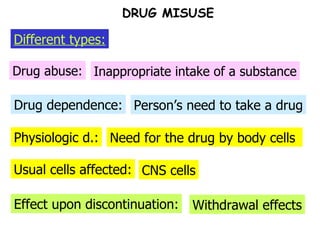
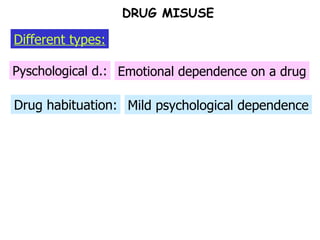
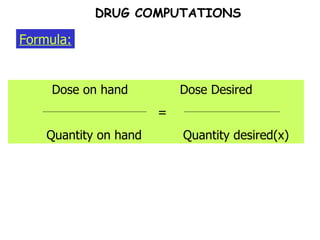
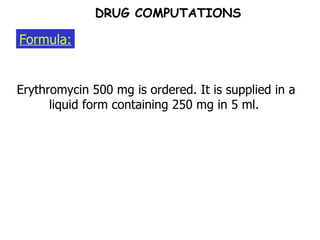
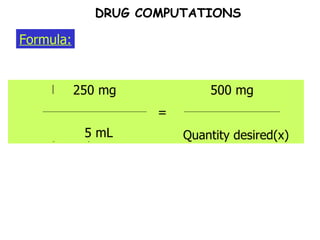
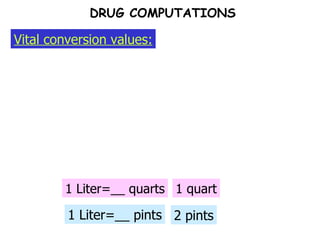
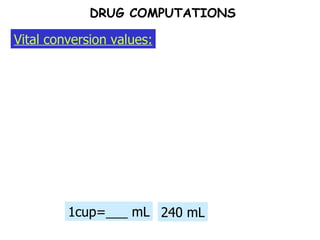
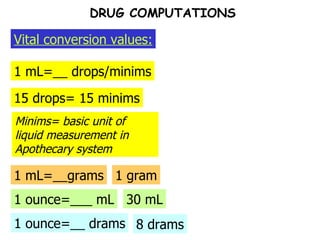
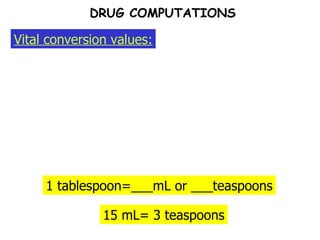
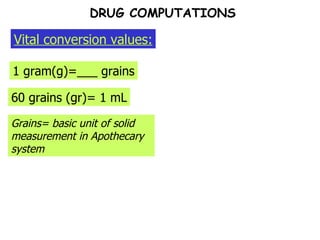
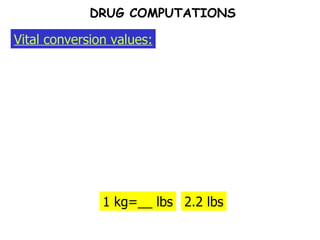
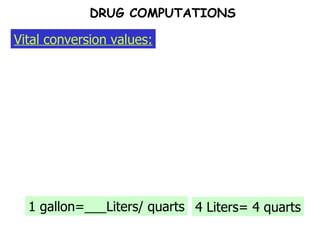
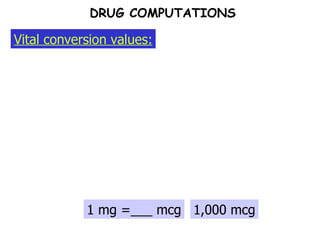
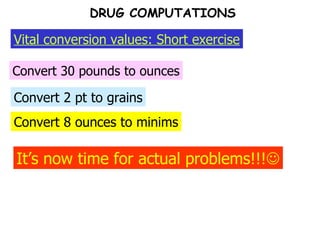
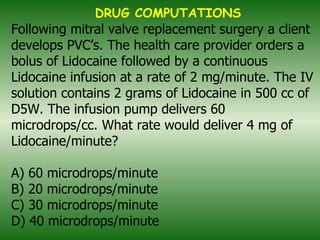
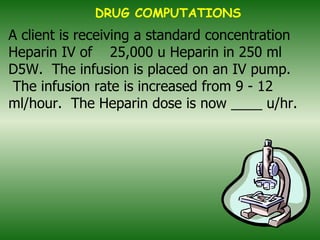
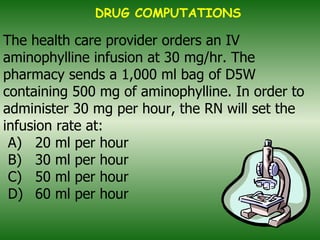
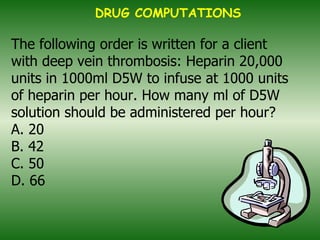
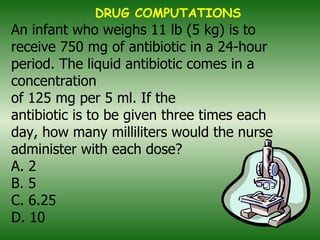
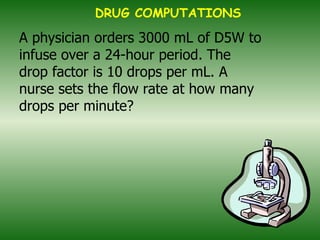
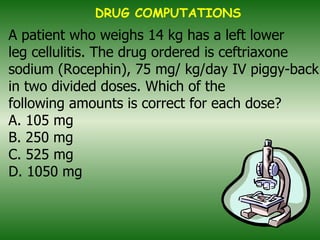
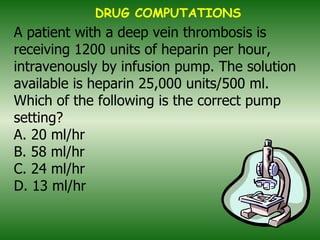
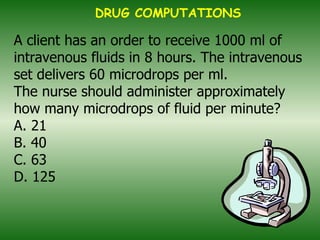
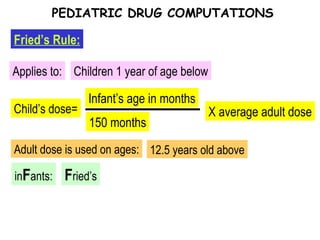
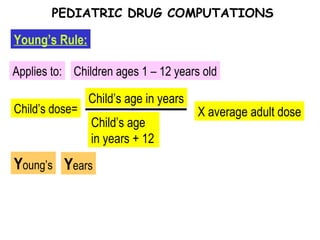
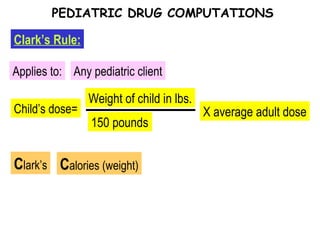
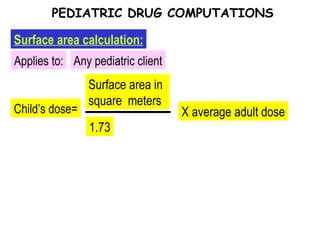
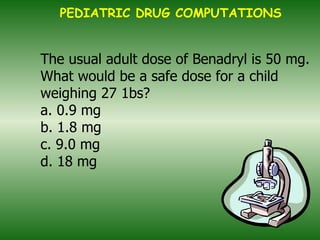
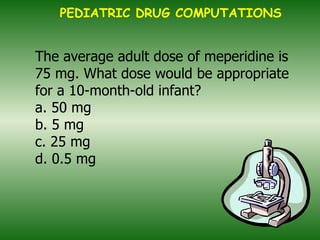
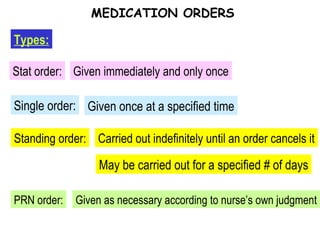
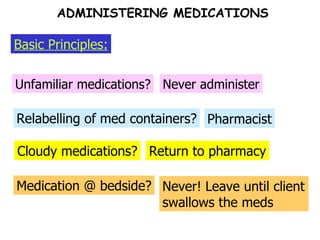
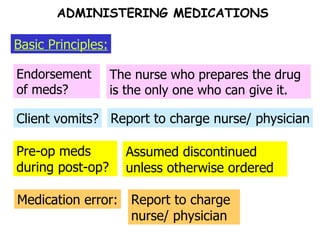
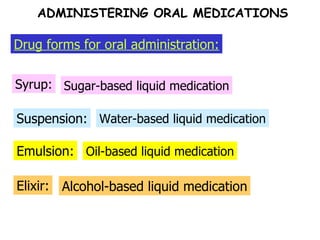
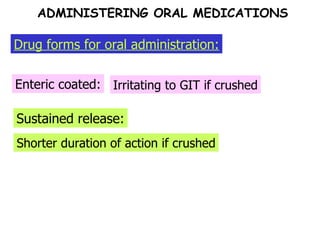
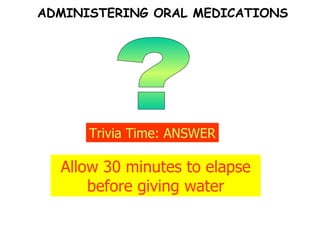
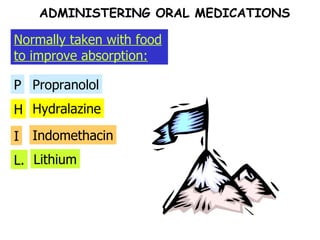
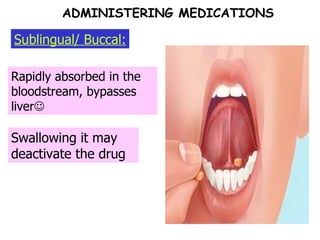
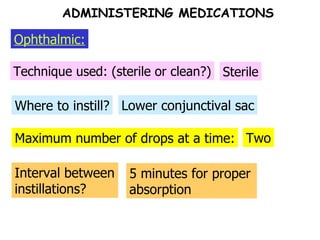
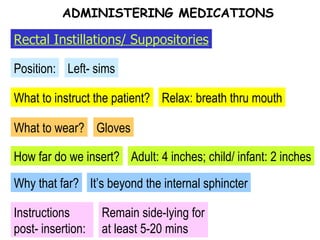
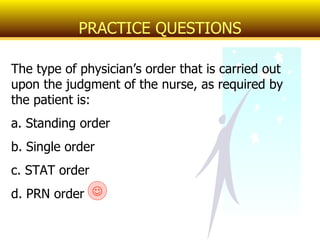
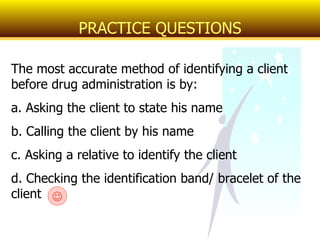
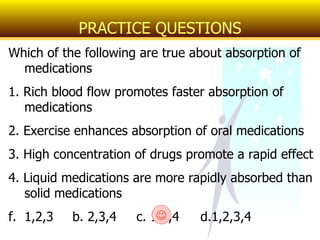
This document provides an overview of pharmacology basics including definitions of key terms, drug categories, pharmacodynamics, pharmacokinetics, drug computations, and examples of nursing teachings related to over-the-counter medications and sample patient cases. Key concepts covered include drug absorption, distribution, metabolism, excretion, factors influencing drug effects, allergic reactions, and conversions between units of measurement for drug dosages.