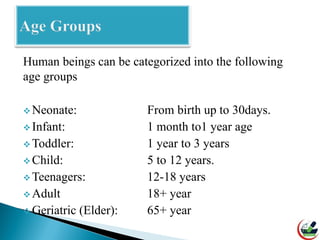
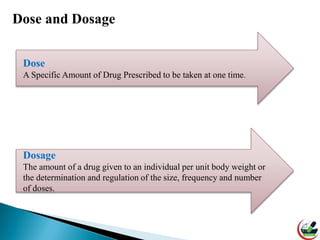
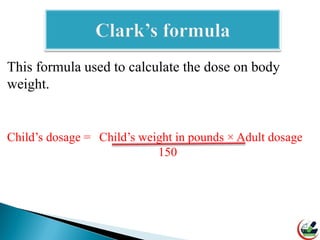
Pharmacology deals with determining safe and effective drug doses based on various patient factors. Dose calculations consider age, weight, disease states, drug interactions, and other variables. Special care must be taken when dosing pediatric patients, geriatric patients, and women. Three common formulas - Clark's rule, Fried's rule, and Young's rule - are used to calculate appropriate pediatric doses based on age, weight, or available information. Pharmacy technicians must understand dose calculations to accurately dispense and advise on medication use.