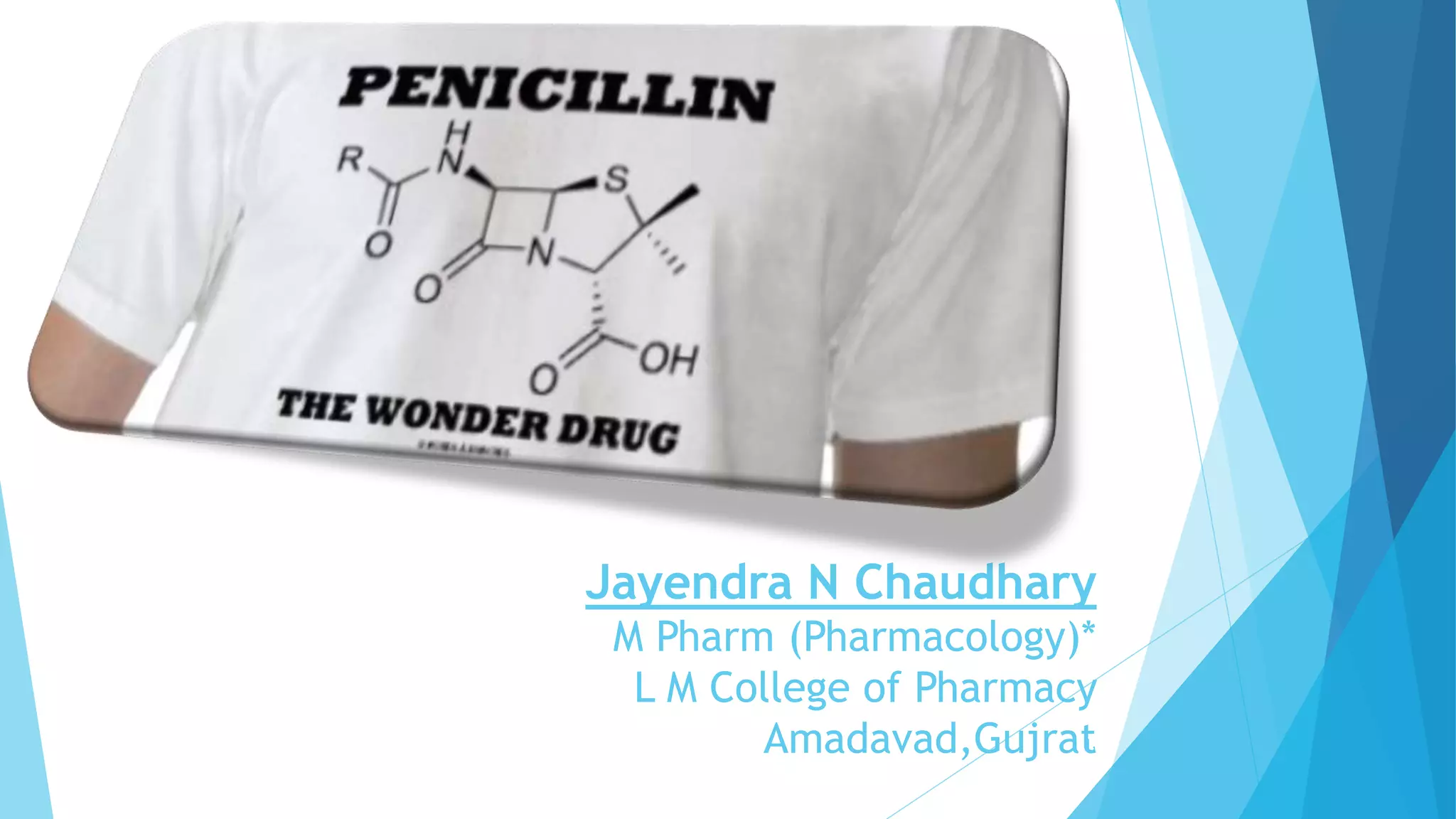
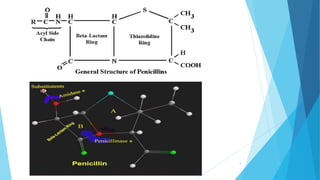
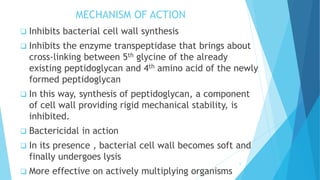
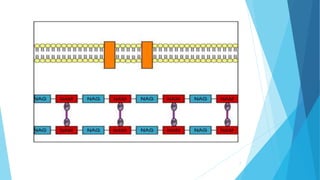
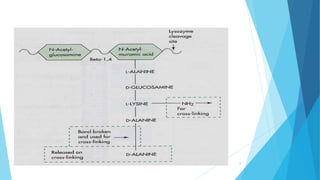
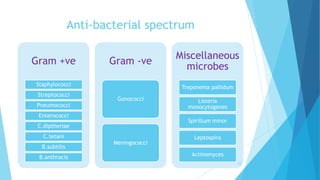
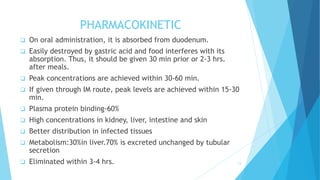
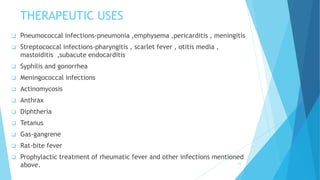
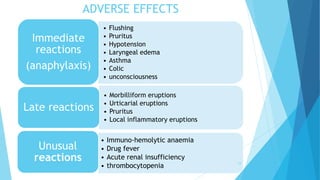
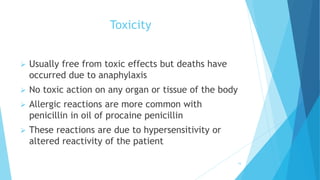
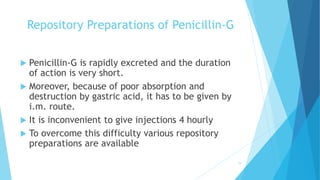
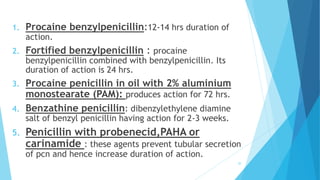
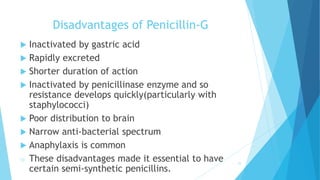
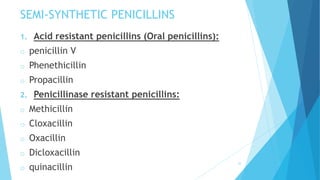
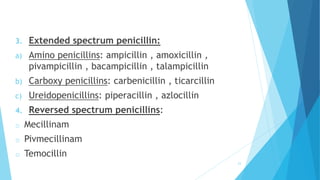
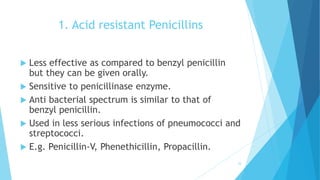
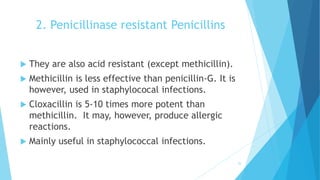
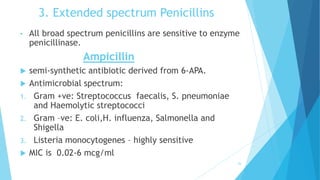
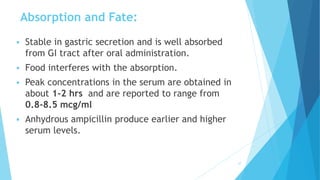
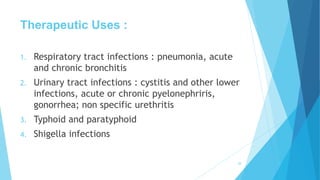
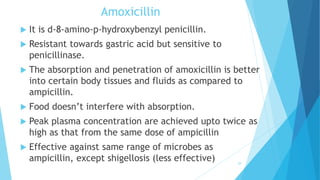
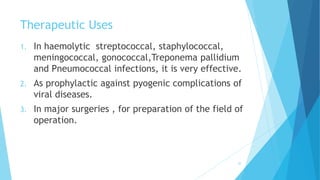
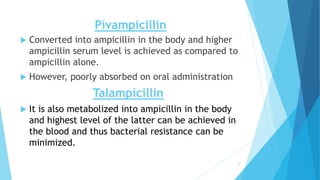
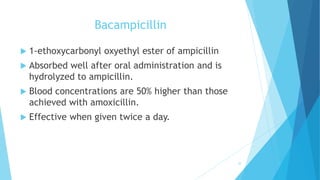
This document discusses penicillin, the first antibiotic discovered by Alexander Fleming in 1928. It was first extracted from the Penicillium mold. Later, Penicillium chrysogenum was found to give the highest yield and is now used to produce penicillin via fermentation. The main types discussed are penicillin G, acid resistant penicillins, penicillinase resistant penicillins, and extended spectrum penicillins. The document covers the mechanism of action, uses, advantages, disadvantages, and side effects of various penicillin derivatives.