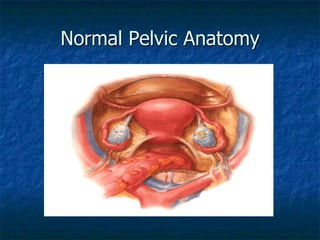
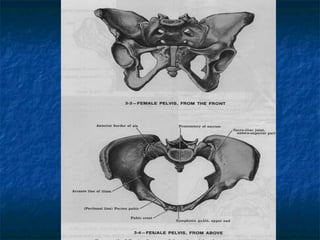
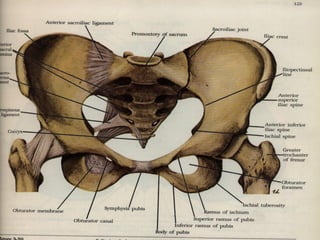
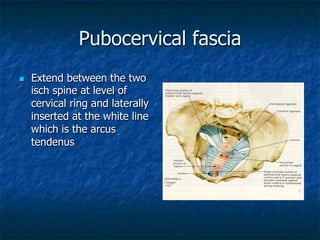
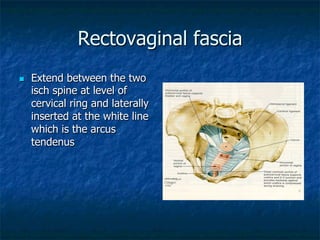
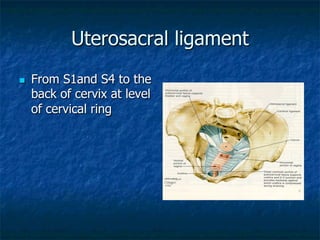
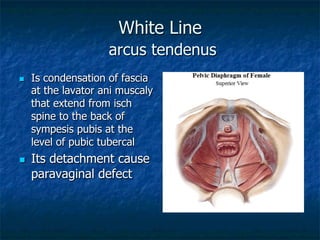
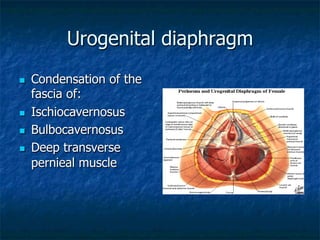
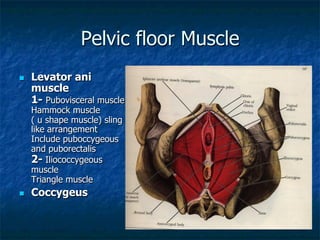
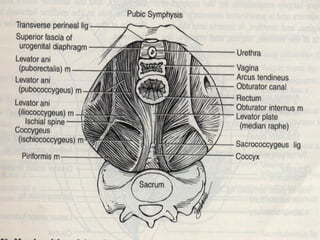
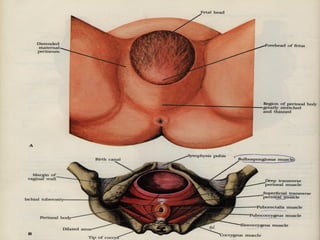
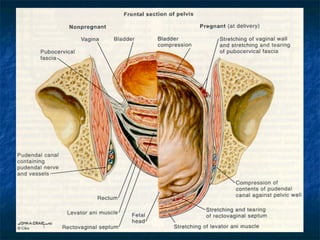
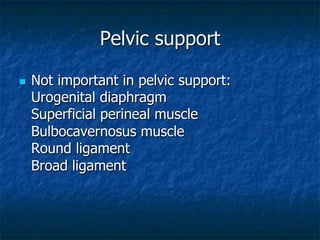
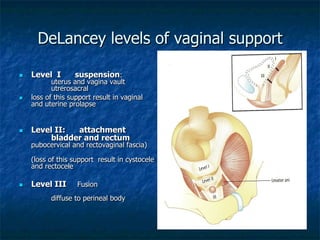
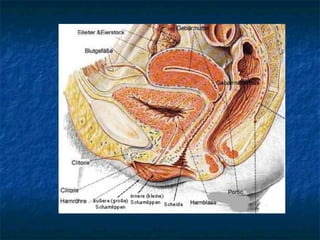
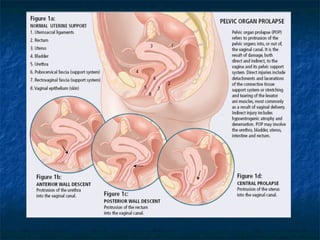
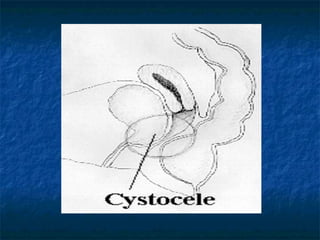
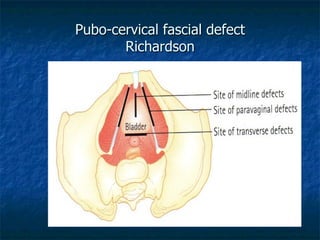
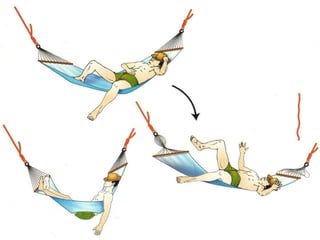
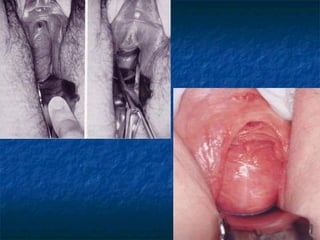
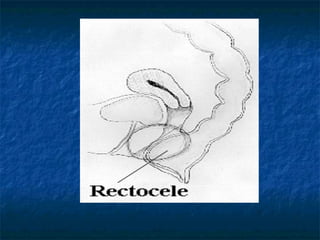
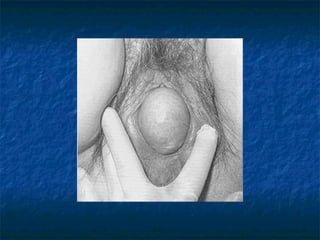
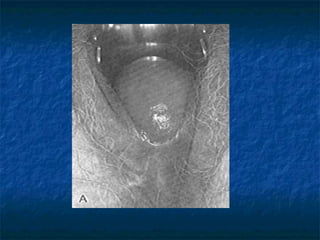
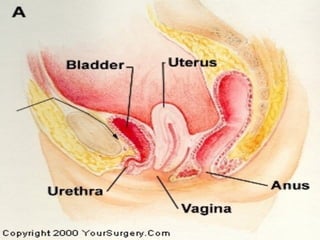
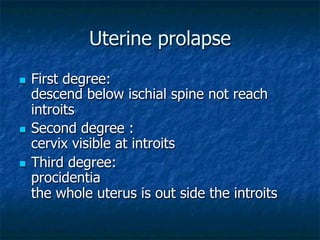
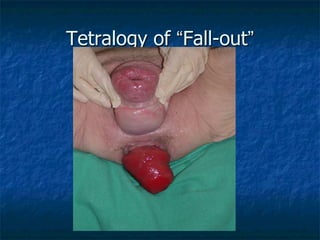
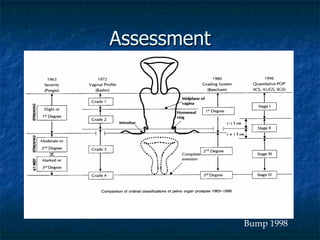
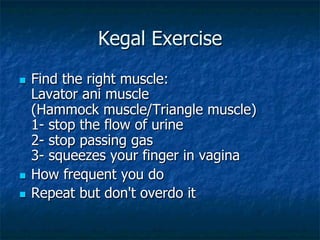
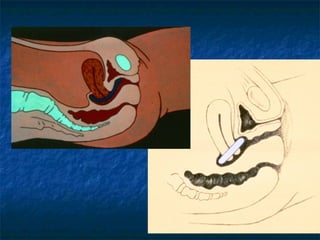
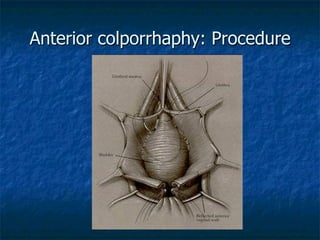
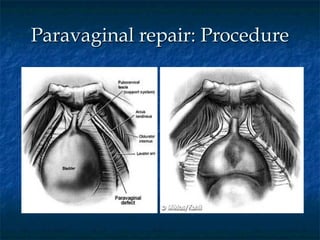
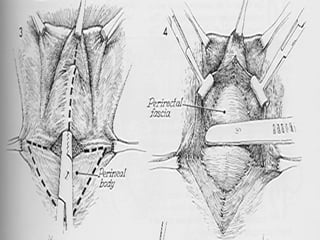
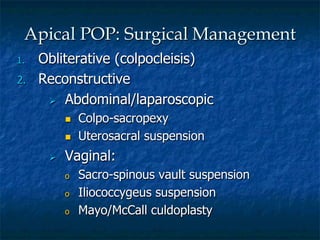
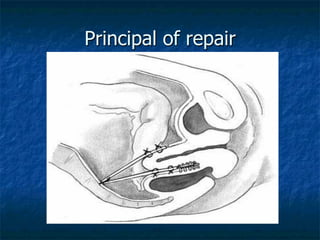
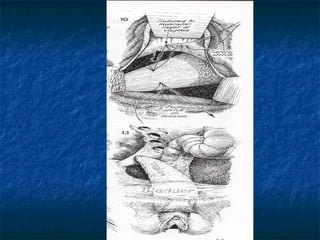
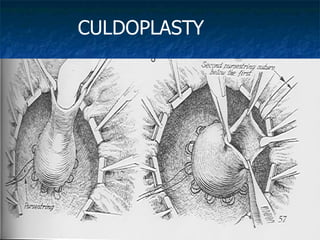
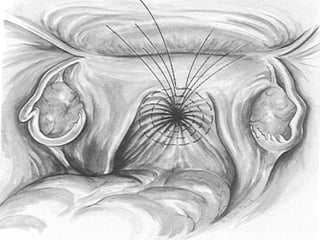
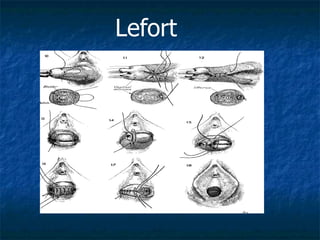
This document discusses pelvic floor dysfunction and pelvic organ prolapse. It begins by describing normal pelvic anatomy including ligaments, tendons, fascia and muscles that provide support. Three levels of vaginal support are identified. Pelvic organ prolapse is then defined as the protrusion of pelvic organs into or outside the vaginal canal. Etiology and risk factors for pelvic organ prolapse are outlined. Assessment, symptoms, and conservative and surgical management options are reviewed for anterior, posterior, and apical prolapse. Surgical procedures including anterior and posterior colporrhaphy, paravaginal repair, and abdominal, laparoscopic and vaginal vault suspension techniques are described.