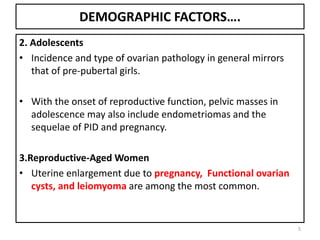
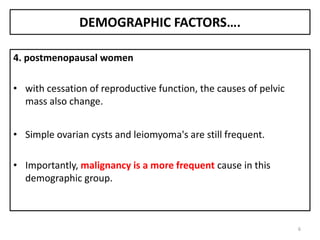
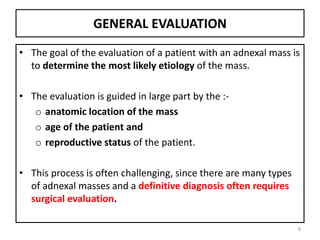
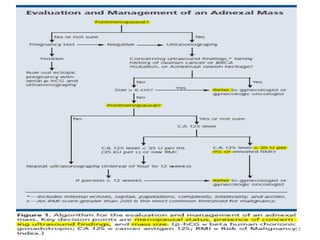
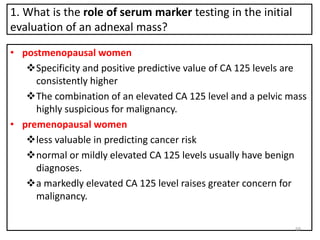
1. The document discusses the evaluation and management of pelvic masses. It covers demographic factors, differential diagnosis, general evaluation including medical history, physical exam, imaging and labs.
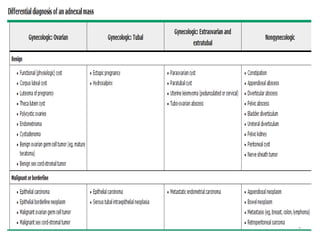
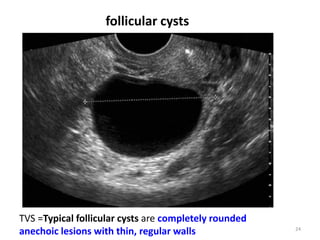
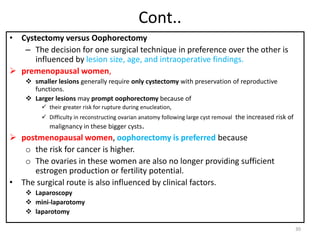
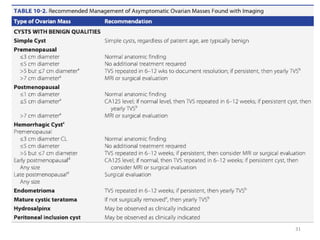
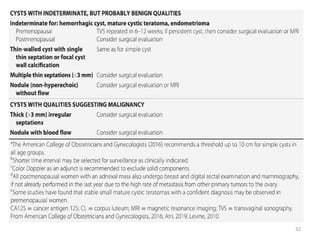
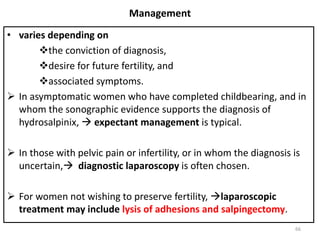
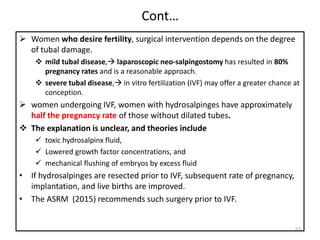
2. Common adnexal masses include functional cysts, dermoid cysts, endometriomas and leiomyomas. Management depends on age, size, symptoms and surgical findings.
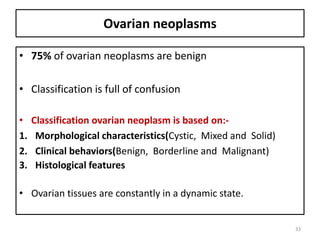
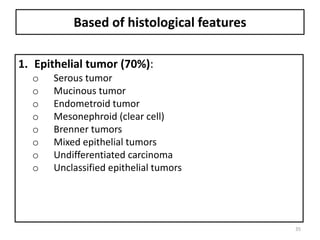
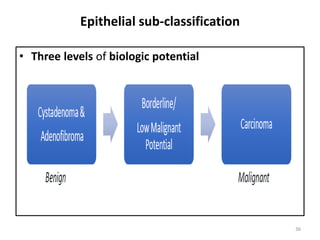
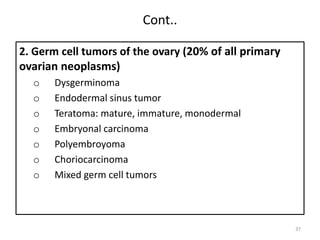
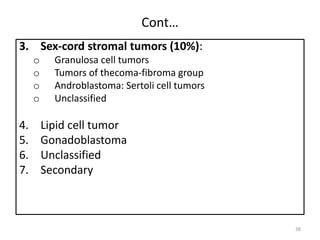
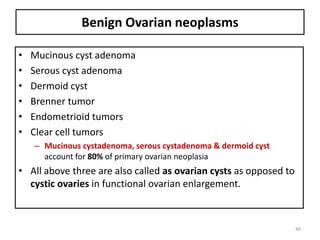
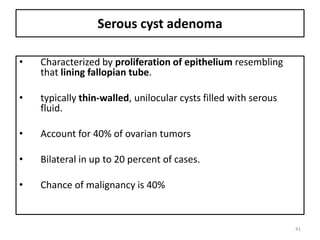
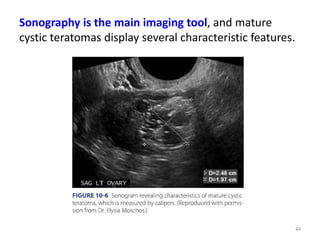
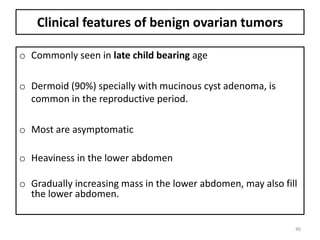
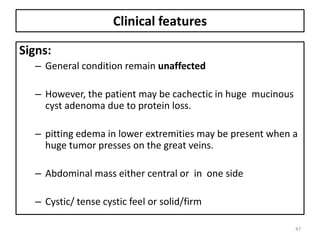
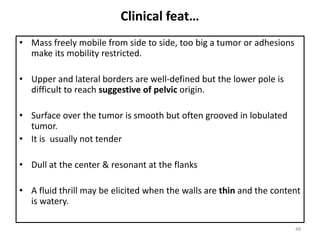
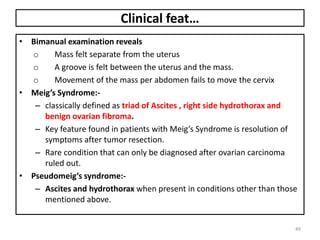
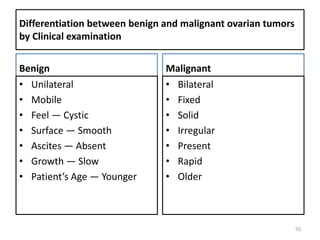
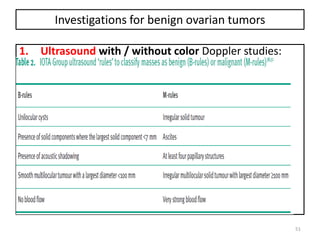
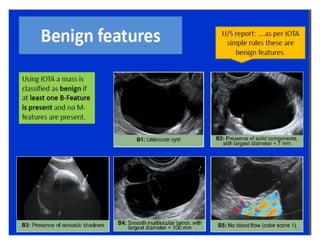
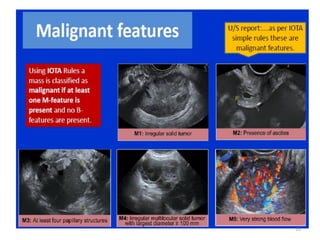
3. Benign ovarian tumors are more common than malignant. Common benign types are serous cyst adenomas, mucinous cyst adenomas and dermoid cysts. Their features, diagnosis and treatment are outlined.