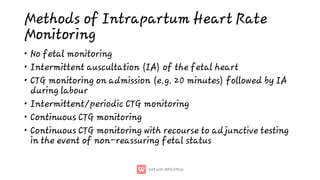
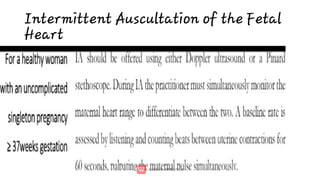
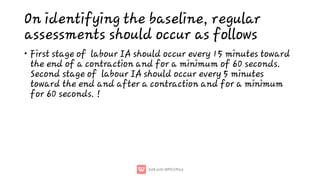
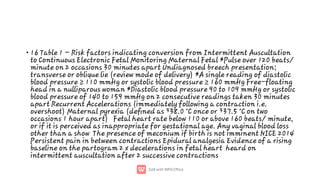
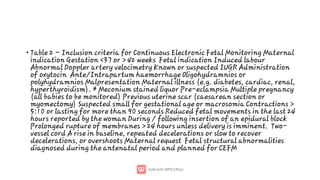
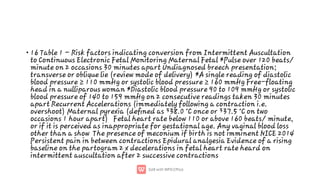
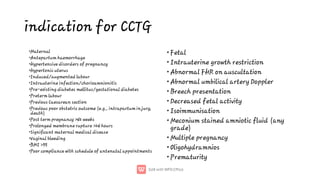
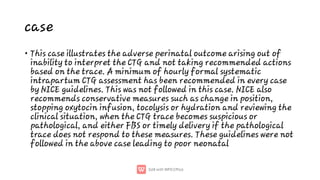
This document discusses intrapartum fetal monitoring methods and guidelines. It describes the purpose of intrapartum surveillance as timely detection of hypoxic babies to prevent morbidity or mortality. Methods discussed include intermittent auscultation of the fetal heart and continuous cardiotocography (CTG) monitoring. Risk factors requiring conversion from intermittent to continuous monitoring are provided. Indications for continuous CTG monitoring include various maternal and fetal conditions. Guidelines for intermittent auscultation and interpreting CTG traces are also summarized, with a case example provided to illustrate the importance of adhering to monitoring guidelines.