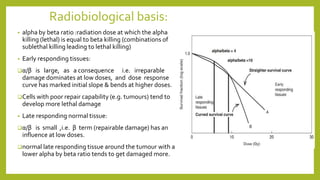
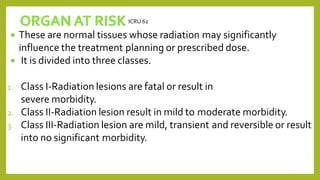
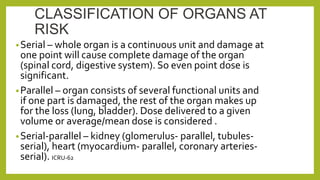
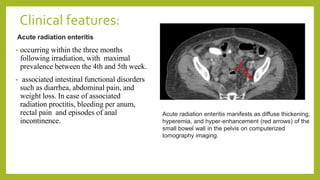
The document discusses classifications of mammalian cell sensitivity to radiation and the radiobiological basis of radiation-induced toxicities. It then focuses on the rectum as an organ at risk for pelvic irradiation, describing the acute and chronic effects of radiation proctitis. Techniques to reduce rectal toxicity during radiotherapy planning and treatment are also outlined, including emptying the rectum during simulation and using rectal spacers or balloons.