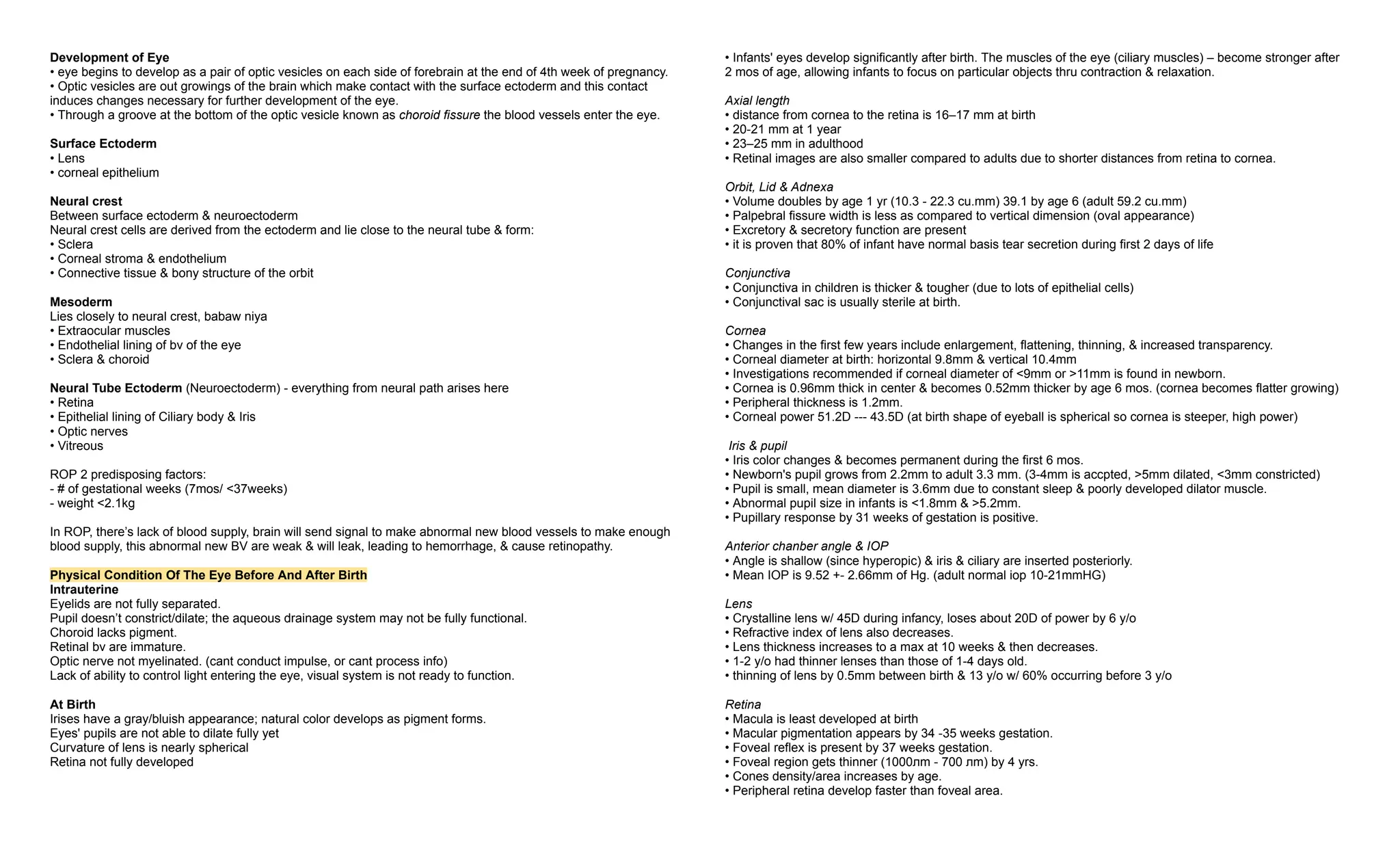
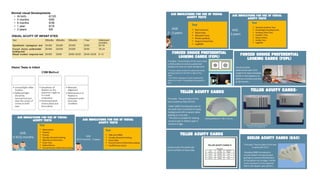
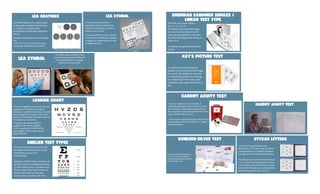
The document provides an overview of the development of the human eye from embryonic stages through early childhood, detailing key milestones such as the formation of optic vesicles, lens development, and retinal maturation. It emphasizes the gradual improvement of vision in infants within the first year, including coordination of eye movements and increased visual acuity. Additionally, it outlines normal visual development phases and the importance of monitoring for potential vision problems during infancy and early childhood.