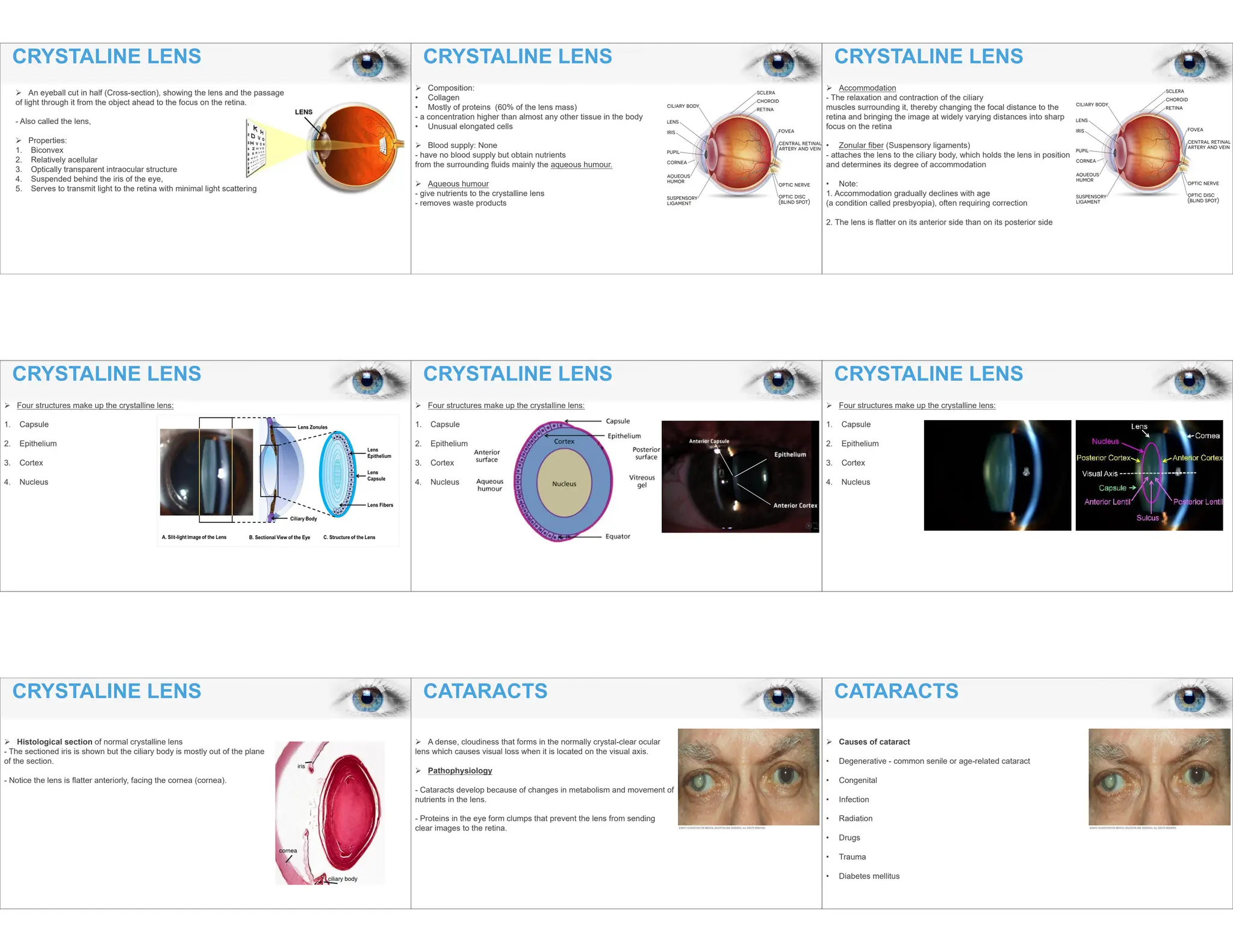
The document provides an in-depth overview of the crystalline lens in the human eye, detailing its structure, function, and involvement in vision, particularly in relation to cataracts. Various types of cataracts are discussed, including their causes, symptoms, and the impact on vision, along with potential surgical treatments such as phacoemulsification and femtosecond laser-assisted procedures. It emphasizes the significance of cataracts as a major cause of visual impairment and outlines the clinical progression and management strategies associated with this condition.