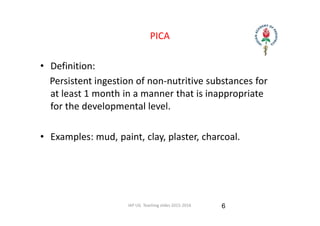
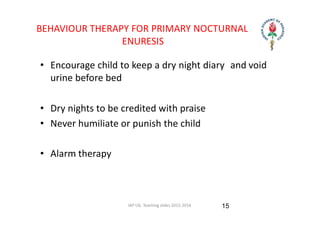
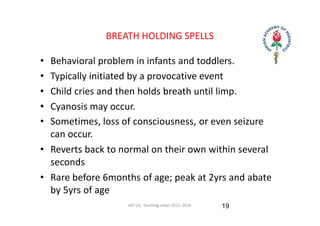
This document summarizes several common behavioral problems in children, including eating disorders like anorexia nervosa and bulimia, pica, bedwetting, thumb sucking, breath holding spells, temper tantrums, tics, teeth grinding, and fecal incontinence. It describes characteristics, causes, and management strategies for each issue. Behavioral problems are often due to developmental delays, stress, neglect, or family dysfunction, and treatment involves addressing underlying causes, behavioral therapy, and sometimes medication.