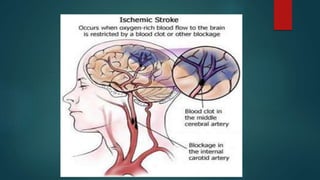
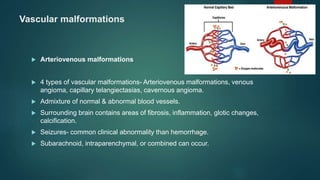
Strokes can occur in children and are usually caused by arterial blockages or venous clots. The incidence of arterial ischemic stroke and cerebral venous thrombosis is approximately 5 per 100,000 children per year. While relatively rare in children, strokes are an important cause of acquired brain injury in newborns and children. The main causes of pediatric strokes include congenital heart defects, infections, vascular abnormalities, genetic conditions, and trauma.