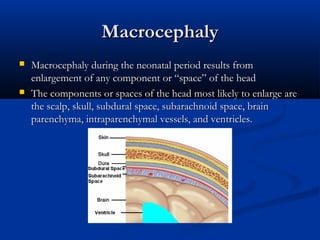
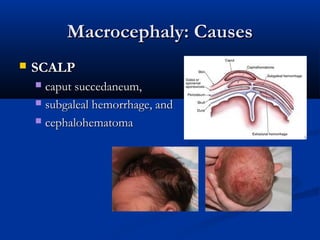
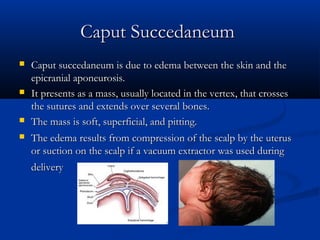
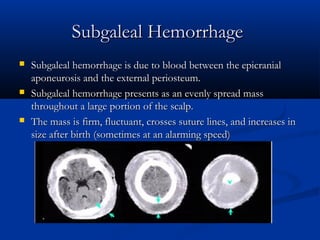
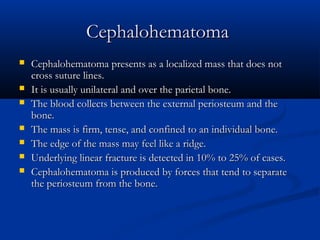
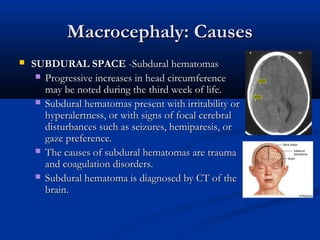
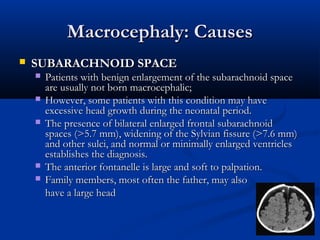
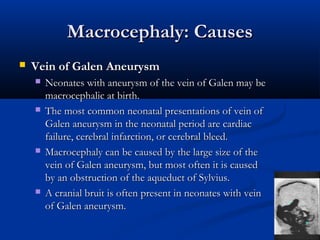
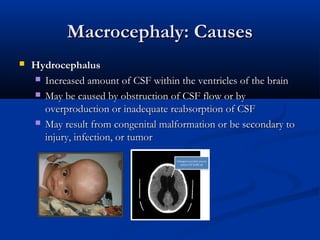
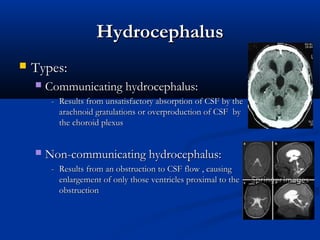
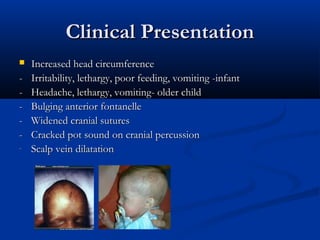
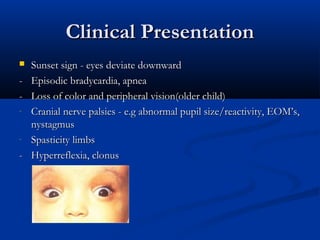
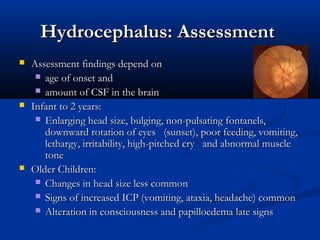
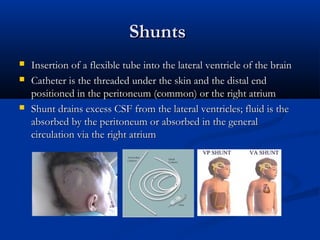
This document discusses various neurological conditions and diseases that can cause macrocephaly in infants and children. It describes conditions present at birth such as caput succedaneum, subgaleal hemorrhage, cephalohematoma, osteopetrosis, subdural hematomas, benign enlargement of the subarachnoid space, megalencephaly, vein of Galen aneurysm, and hydrocephalus. Hydrocephalus and its causes, clinical presentation, assessment, treatments including shunts, and complications are discussed in detail. Posthemorrhagic hydrocephalus as a consequence of intraventricular hemorrhage is also outlined.